Sunday Poster Session
Category: Liver
P1032 - Acute Liver Failure Secondary to Diffuse Large B-Cell Lymphoma Discovered on Explant Pathology; A Rare Case of Survival
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Brian Hughes, MD
University of Colorado-Anschutz Campus
Aurora, CO
Presenting Author(s)
Brian Hughes, MD, Timothy McGinnis, MD, Whitney Jackson, MD
University of Colorado-Anschutz Campus, Aurora, CO
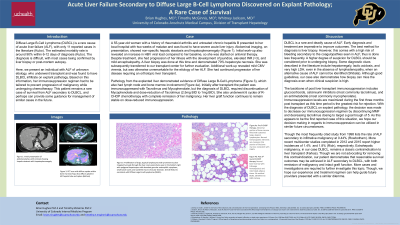
Introduction: Diffuse Large B-Cell Lymphoma (DLBCL) is a rare cause of acute liver failure (ALF), with only 11 reported cases in the literature. The estimated mortality rate is around 90% within 6-12 days of diagnosis. Here, we present an individual with ALF of unknown etiology, who underwent transplant and was found to have DLBCL infiltrate on explant pathology. Based on this information, the immunosuppression regimen was tailored to prevent progression of malignancy while undergoing chemotherapy. This patient remains a rare case of survival from ALF secondary to DLBCL and can provide guidance for management of similar cases.
Case Description/Methods: A 55-year-old woman with a history of untreated chronic hepatitis B presented with two weeks of malaise and was found to have acute liver injury. Initial work-up revealed an increase in HBV viral load compared to her baseline, so she was started on antiviral therapy. Despite treatment, she had progression of her illness to acute liver failure. A liver biopsy done at this time demonstrated 70% hepatocyte necrosis. Additional work-up revealed mild CMV viremia, but was otherwise unremarkable for the etiology of her ALF. She had continued progression of her disease requiring an orthotopic liver transplant. Pathology from the explanted liver demonstrated evidence of DLBCL, which also had lymph node and bone marrow involvement. Initially after transplant the patient was immunosuppressed with Tacrolimus and Mycophenolate, but the diagnosis of DLBCL required discontinuation of Mycophenolate and dose-reduction of Tacrolimus (2.5mg BID to 1mg BID). She underwent 6 cycles of R-CHOP chemotherapy with complete remission of her malignancy. Her liver graft function continues to remain stable on dose-reduced immunosuppression at least 6 months post diagnosis.
Discussion: DLBCL is a rare and deadly cause of ALF. Early diagnosis and treatment is imperative to improve outcomes. However, the best method of diagnosis is biopsy which comes with increased risk of bleeding from coagulopathies seen in ALF, thus is done less frequently. We suggest further consideration for biopsy when there is a higher suspicion of DLBCL (hepatomegaly, lactic acidosis, and very high LDH, even in the absence of lymphadenopathy) when an alternative cause of ALF cannot be identified. Our case presents one example of both cancer remission and graft survival post-transplant with an individualized treatment regimen which could be used for future patients.
Disclosures:
Brian Hughes, MD, Timothy McGinnis, MD, Whitney Jackson, MD. P1032 - Acute Liver Failure Secondary to Diffuse Large B-Cell Lymphoma Discovered on Explant Pathology; A Rare Case of Survival, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
University of Colorado-Anschutz Campus, Aurora, CO
Introduction: Diffuse Large B-Cell Lymphoma (DLBCL) is a rare cause of acute liver failure (ALF), with only 11 reported cases in the literature. The estimated mortality rate is around 90% within 6-12 days of diagnosis. Here, we present an individual with ALF of unknown etiology, who underwent transplant and was found to have DLBCL infiltrate on explant pathology. Based on this information, the immunosuppression regimen was tailored to prevent progression of malignancy while undergoing chemotherapy. This patient remains a rare case of survival from ALF secondary to DLBCL and can provide guidance for management of similar cases.
Case Description/Methods: A 55-year-old woman with a history of untreated chronic hepatitis B presented with two weeks of malaise and was found to have acute liver injury. Initial work-up revealed an increase in HBV viral load compared to her baseline, so she was started on antiviral therapy. Despite treatment, she had progression of her illness to acute liver failure. A liver biopsy done at this time demonstrated 70% hepatocyte necrosis. Additional work-up revealed mild CMV viremia, but was otherwise unremarkable for the etiology of her ALF. She had continued progression of her disease requiring an orthotopic liver transplant. Pathology from the explanted liver demonstrated evidence of DLBCL, which also had lymph node and bone marrow involvement. Initially after transplant the patient was immunosuppressed with Tacrolimus and Mycophenolate, but the diagnosis of DLBCL required discontinuation of Mycophenolate and dose-reduction of Tacrolimus (2.5mg BID to 1mg BID). She underwent 6 cycles of R-CHOP chemotherapy with complete remission of her malignancy. Her liver graft function continues to remain stable on dose-reduced immunosuppression at least 6 months post diagnosis.
Discussion: DLBCL is a rare and deadly cause of ALF. Early diagnosis and treatment is imperative to improve outcomes. However, the best method of diagnosis is biopsy which comes with increased risk of bleeding from coagulopathies seen in ALF, thus is done less frequently. We suggest further consideration for biopsy when there is a higher suspicion of DLBCL (hepatomegaly, lactic acidosis, and very high LDH, even in the absence of lymphadenopathy) when an alternative cause of ALF cannot be identified. Our case presents one example of both cancer remission and graft survival post-transplant with an individualized treatment regimen which could be used for future patients.
Disclosures:
Brian Hughes indicated no relevant financial relationships.
Timothy McGinnis indicated no relevant financial relationships.
Whitney Jackson indicated no relevant financial relationships.
Brian Hughes, MD, Timothy McGinnis, MD, Whitney Jackson, MD. P1032 - Acute Liver Failure Secondary to Diffuse Large B-Cell Lymphoma Discovered on Explant Pathology; A Rare Case of Survival, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
