Sunday Poster Session
Category: Liver
P1037 - Metastatic Breast Cancer Presenting as Obstructive Jaundice
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Aleena Moin, DO
Geisinger Medical Center
Danville, PA
Presenting Author(s)
Aleena Moin, DO1, Harrison Reid Malcolm, DO2, Nicole Anderson, DO1, Olivia Granja, MS3, Harshit S. Khara, MD1, Alberto Unzueta, MD1
1Geisinger Medical Center, Danville, PA; 2Geisinger Health System, Danville, PA; 3Geisinger Commonwealth School of Medicine, Danville, PA
Introduction: Breast cancer represents 15% of all new female cancers in the United States, with nearly 6% of patients having invasive breast cancer at diagnosis. The liver is the third most common site of metastasis. Diagnosis of hepatic metastasis is usually supported by imaging. We present a rare case of recurrent breast cancer with hepatic metastasis, not previously seen in imaging studies, detected after a liver biopsy.
Case Description/Methods: A 49-year-old female with a history of triple-negative, BRCA-1-associated breast cancer status post neoadjuvant chemotherapy, bilateral mastectomy, and adjuvant radiation (in complete remission for two years) presented to the gastroenterology clinic for evaluation of elevated liver enzymes consistent with obstructive jaundice. Laboratory evaluation was as follows: AST 119 U/L, ALT 43 U/L, Alkaline Phos 305 U/L, total bilirubin 4.1, direct bilirubin 3.5, GGTP 1047 U/L, and INR 1.0. Workup for acute viral hepatitis, HIV, HSV, and CMV was negative, but EBV IgM/IgG titers were positive. Autoimmune studies, including ANA, AMA, and anti-smooth muscle antibodies were negative. Imaging with computed tomography and magnetic resonance imaging (MRI) of the abdomen/pelvis was unremarkable. At this time, the differential included EBV hepatitis.
Later, the patient developed severe pancytopenia with resulting bone marrow biopsy showing hypercellularity with concern for metastatic disease. Histologic assessment for persistent liver enzyme elevation and jaundice was pursued with a trans-jugular liver biopsy. Pathology noted pleomorphic tumor cells consistent with metastatic carcinoma, favoring primary breast cancer. The patient was referred to oncology for palliative treatment with chemotherapy and radiation.
Discussion: Our case demonstrates a unique example of metastatic breast cancer noted after liver biopsy. Obstructive jaundice was likely secondary to sinusoidal obstruction from malignant cells. Positive EBV serology was a red herring in this case and did not explain the patient’s rising liver enzymes. Lack of imaging findings does not rule out metastatic disease. Histologic evaluation should be considered in patients with history of malignancy without explainable cause for persistent liver derangements.

Disclosures:
Aleena Moin, DO1, Harrison Reid Malcolm, DO2, Nicole Anderson, DO1, Olivia Granja, MS3, Harshit S. Khara, MD1, Alberto Unzueta, MD1. P1037 - Metastatic Breast Cancer Presenting as Obstructive Jaundice, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Geisinger Medical Center, Danville, PA; 2Geisinger Health System, Danville, PA; 3Geisinger Commonwealth School of Medicine, Danville, PA
Introduction: Breast cancer represents 15% of all new female cancers in the United States, with nearly 6% of patients having invasive breast cancer at diagnosis. The liver is the third most common site of metastasis. Diagnosis of hepatic metastasis is usually supported by imaging. We present a rare case of recurrent breast cancer with hepatic metastasis, not previously seen in imaging studies, detected after a liver biopsy.
Case Description/Methods: A 49-year-old female with a history of triple-negative, BRCA-1-associated breast cancer status post neoadjuvant chemotherapy, bilateral mastectomy, and adjuvant radiation (in complete remission for two years) presented to the gastroenterology clinic for evaluation of elevated liver enzymes consistent with obstructive jaundice. Laboratory evaluation was as follows: AST 119 U/L, ALT 43 U/L, Alkaline Phos 305 U/L, total bilirubin 4.1, direct bilirubin 3.5, GGTP 1047 U/L, and INR 1.0. Workup for acute viral hepatitis, HIV, HSV, and CMV was negative, but EBV IgM/IgG titers were positive. Autoimmune studies, including ANA, AMA, and anti-smooth muscle antibodies were negative. Imaging with computed tomography and magnetic resonance imaging (MRI) of the abdomen/pelvis was unremarkable. At this time, the differential included EBV hepatitis.
Later, the patient developed severe pancytopenia with resulting bone marrow biopsy showing hypercellularity with concern for metastatic disease. Histologic assessment for persistent liver enzyme elevation and jaundice was pursued with a trans-jugular liver biopsy. Pathology noted pleomorphic tumor cells consistent with metastatic carcinoma, favoring primary breast cancer. The patient was referred to oncology for palliative treatment with chemotherapy and radiation.
Discussion: Our case demonstrates a unique example of metastatic breast cancer noted after liver biopsy. Obstructive jaundice was likely secondary to sinusoidal obstruction from malignant cells. Positive EBV serology was a red herring in this case and did not explain the patient’s rising liver enzymes. Lack of imaging findings does not rule out metastatic disease. Histologic evaluation should be considered in patients with history of malignancy without explainable cause for persistent liver derangements.

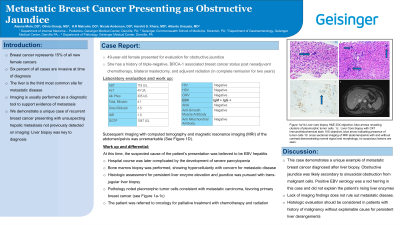
Figure: Figure 1a/1b Liver core biopsy H&E 20X objective, blue arrows revealing clusters of pleomorphic tumor cells. 1c: Liver Core biopsy with CK7 immunohistochemical stain 10X objective, a blue arrow indicating presence of tumor cells 1d: cross-sectional imaging of MRI abdomen/pelvis with and without contrast demonstrating normal signal and morphology, no suspicious lesions are seen.
Disclosures:
Aleena Moin indicated no relevant financial relationships.
Harrison Reid Malcolm indicated no relevant financial relationships.
Nicole Anderson indicated no relevant financial relationships.
Olivia Granja indicated no relevant financial relationships.
Harshit Khara: Boston Scientific – Consultant, Speakers Bureau. Castle Biosciences – Consultant, Speakers Bureau. ConMed – Consultant, Speakers Bureau. Cook Medical – Consultant, Speakers Bureau. Medtronic – Consultant, Speakers Bureau. Olympus America – Consultant, Speakers Bureau. Pentax – Consultant, Speakers Bureau.
Alberto Unzueta indicated no relevant financial relationships.
Aleena Moin, DO1, Harrison Reid Malcolm, DO2, Nicole Anderson, DO1, Olivia Granja, MS3, Harshit S. Khara, MD1, Alberto Unzueta, MD1. P1037 - Metastatic Breast Cancer Presenting as Obstructive Jaundice, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
