Sunday Poster Session
Category: Liver
P1039 - Fulminant Liver Failure from Hepatitis E in an Immunocompetent Adult
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio
- JG
Jason Goldenberg, MD
Thomas Jefferson University Hospital
Philadelphia, PA
Presenting Author(s)
Jason Goldenberg, MD, Joshua Riley, MD, Rebecca Loh, MD, David Strayer, MD, PhD, Elizaveta Flerova, MD, Jesse Civan, MD
Thomas Jefferson University Hospital, Philadelphia, PA
Introduction: Hepatitis E Virus (HEV) is a common cause of acute hepatitis worldwide, but a very rare cause of acute liver failure in the United States that has typically been limited to individuals with diabetes mellitus and acute myeloid leukemia. This case report details an immunocompetent individual without travel history that suffered fatal fulminant liver failure from acute Hepatitis E.
Case Description/Methods: A 79-year-old gentleman with history of CAD, hypothyroidism, remote history of resolved hepatitis A, and uncomplicated COVID infection 1 month prior was transferred to our institution due to worsening mental status.
He originally presented to his local hospital with weeks of weight loss and anorexia with acute change in mentation. He was found to have AST 1755, ALT 2007, ferritin >1500, INR >17.8, with undetectable acetaminophen and ethanol levels. Liver ultrasound demonstrated normal liver echogenicity without evidence of portal vein thrombus. CT head was unremarkable. He was subsequently transferred to our institution for acute liver failure.
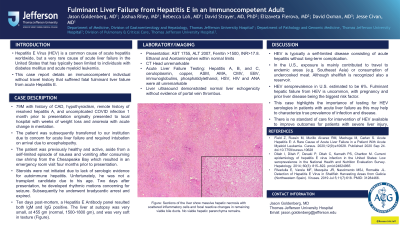
Upon arrival he required intubation due to mental status. Family noted he had been previously healthy and active, aside from food poisoning after consuming raw shrimp 4 months prior to presentation. They denied any new medications, supplements, recent travel or sick contacts. He was treated with empiric N-Acetyl Cysteine and supportive care. Further laboratory evaluation including Hepatitis A, B, and C, ceruloplasmin, copper, ASM, AMA, CMV, EBV, immunoglobulins, phosphatidylethanol, HSV, HIV and ANA were all unremarkable. Steroids were not initiated. He was deemed not a transplant candidate due to his age. Unfortunately, he passed from progressive multisystem organ failure. Ten days post mortem, a Hepatitis E Antibody panel resulted both IgM and IgG positive. The liver at autopsy was very small, at 455 gm (normal, 1500-1800 gm), and was very soft in texture(Figure).
Discussion: HEV is typically a self-limited disease consisting of acute hepatitis without long-term complication. In the U.S., exposure is mainly contributed to travel to endemic areas (e.g. Southeast Asia) or consumption of undercooked meat. HEV seroprevalence in U.S. estimated to be 6%. Fulminant hepatic failure from HEV is uncommon, with pregnancy and prior liver disease being the biggest risk factor. Although identifying the etiology of ALF is important, there remains no established therapeutic intervention to improve chances of transplant-free survival.

Disclosures:
Jason Goldenberg, MD, Joshua Riley, MD, Rebecca Loh, MD, David Strayer, MD, PhD, Elizaveta Flerova, MD, Jesse Civan, MD. P1039 - Fulminant Liver Failure from Hepatitis E in an Immunocompetent Adult, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Thomas Jefferson University Hospital, Philadelphia, PA
Introduction: Hepatitis E Virus (HEV) is a common cause of acute hepatitis worldwide, but a very rare cause of acute liver failure in the United States that has typically been limited to individuals with diabetes mellitus and acute myeloid leukemia. This case report details an immunocompetent individual without travel history that suffered fatal fulminant liver failure from acute Hepatitis E.
Case Description/Methods: A 79-year-old gentleman with history of CAD, hypothyroidism, remote history of resolved hepatitis A, and uncomplicated COVID infection 1 month prior was transferred to our institution due to worsening mental status.
He originally presented to his local hospital with weeks of weight loss and anorexia with acute change in mentation. He was found to have AST 1755, ALT 2007, ferritin >1500, INR >17.8, with undetectable acetaminophen and ethanol levels. Liver ultrasound demonstrated normal liver echogenicity without evidence of portal vein thrombus. CT head was unremarkable. He was subsequently transferred to our institution for acute liver failure.
Upon arrival he required intubation due to mental status. Family noted he had been previously healthy and active, aside from food poisoning after consuming raw shrimp 4 months prior to presentation. They denied any new medications, supplements, recent travel or sick contacts. He was treated with empiric N-Acetyl Cysteine and supportive care. Further laboratory evaluation including Hepatitis A, B, and C, ceruloplasmin, copper, ASM, AMA, CMV, EBV, immunoglobulins, phosphatidylethanol, HSV, HIV and ANA were all unremarkable. Steroids were not initiated. He was deemed not a transplant candidate due to his age. Unfortunately, he passed from progressive multisystem organ failure. Ten days post mortem, a Hepatitis E Antibody panel resulted both IgM and IgG positive. The liver at autopsy was very small, at 455 gm (normal, 1500-1800 gm), and was very soft in texture(Figure).
Discussion: HEV is typically a self-limited disease consisting of acute hepatitis without long-term complication. In the U.S., exposure is mainly contributed to travel to endemic areas (e.g. Southeast Asia) or consumption of undercooked meat. HEV seroprevalence in U.S. estimated to be 6%. Fulminant hepatic failure from HEV is uncommon, with pregnancy and prior liver disease being the biggest risk factor. Although identifying the etiology of ALF is important, there remains no established therapeutic intervention to improve chances of transplant-free survival.

Figure: Sections of the liver show massive hepatic necrosis with scattered inflammatory cells and focal reactive changes in remaining viable bile ducts. No viable hepatic parenchyma remains.
Disclosures:
Jason Goldenberg indicated no relevant financial relationships.
Joshua Riley indicated no relevant financial relationships.
Rebecca Loh indicated no relevant financial relationships.
David Strayer indicated no relevant financial relationships.
Elizaveta Flerova indicated no relevant financial relationships.
Jesse Civan indicated no relevant financial relationships.
Jason Goldenberg, MD, Joshua Riley, MD, Rebecca Loh, MD, David Strayer, MD, PhD, Elizaveta Flerova, MD, Jesse Civan, MD. P1039 - Fulminant Liver Failure from Hepatitis E in an Immunocompetent Adult, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
