Sunday Poster Session
Category: Liver
P1042 - A Rare Case of Small Hepatic Vein Budd Chiari Syndrome Presenting as an Inferior Vena Cava Obstruction Secondary to Compression by Hypertrophied Caudate Lobe
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio
- AE
Abdelwahap Elghezewi, MD
Marshall University
Huntington, WV
Presenting Author(s)
Abdelwahap Elghezewi, MD1, Mohamed Hammad, MD1, Mujtaba Mohamed, MBBS2, Peter Chirico, MD3, Wesam Frandah, MD3
1Marshall University, Huntington, WV; 2Joan C. Edwards School of Medicine, Huntington, WV; 3Marshall University Joan C. Edwards School of Medicine, Huntington, WV
Introduction: Budd‐Chiari syndrome (BCS) is defined as an obstruction of the hepatic venous outflow in the absence of cardiac or pericardial diseases. Obstruction can occur in large hepatic veins, the supra hepatic portion of the inferior vena cava, or small hepatic veins. It is a very rare condition with an incidence below 1 case per million population. The most common clinical presentation of BCS is ascites (83%) and abdominal pain (61%). Inferior vena cava obstruction is seen as the initial symptom. Diagnosis is usually made by demonstration of hepatic venous flow obstruction by noninvasive imaging techniques (Doppler ultrasonography, CT, or MR). However, imaging studies don’t depict BCS in small hepatic veins since images tend not to reveal hepatic venous obstruction leaving liver biopsy and venography as the last line to confirm the diagnosis.
Case Description/Methods: A 51-year-old woman with no significant PMH presented to the emergency department with acute bilateral leg swelling and abdominal swelling for two weeks. She states she is a healthy person. Physical exam: Vital signs: BP: 100/50 mmHg, HR: 110 BPM. Abdominal exam: massive ascites and lower limb swelling with anasarca. The chest exam is clear. She had a normal comprehensive metabolic panel and a normal complete blood count. The abdominal US showed massive ascites. Ascitic fluid studies showed serum ascites fluid gradient of 2.5. with predominantly lymphocytes (95%). Echocardiogram showed a normal ejection fraction of 60% otherwise completely normal. CT abdomen and MR venography showed caudate lobe enlargement compressing IVC with liver parenchymal changes. A tissue biopsy was obtained by endoscopic ultrasound. The patient was found to have Budd Chiari syndrome. Hypercoagulable workup was positive for JAK-2 mutation. The patient was started on Eliquis, Two weeks following the initiation of antithrombotic treatment patient’s abdominal ascites and lower limb swelling started to improve. Right hepatic stent was placed afterward.
Discussion: Budd-Chiari syndrome (BCS) or hepatic vein thrombosis (HVT), is a rare disorder resulting from obstruction of the hepatic venous outflow. It can present as Inferior vena cava obstruction by an enlarged caudate lobe or clot obstructive the IVC lumen. The diagnostic modality of choice is Doppler US, CT, or MRI. Diagnosis can be challenging in small vein hepatic BCS. Biopsy and venography are reserved as last resort to establish the diagnosis.

Disclosures:
Abdelwahap Elghezewi, MD1, Mohamed Hammad, MD1, Mujtaba Mohamed, MBBS2, Peter Chirico, MD3, Wesam Frandah, MD3. P1042 - A Rare Case of Small Hepatic Vein Budd Chiari Syndrome Presenting as an Inferior Vena Cava Obstruction Secondary to Compression by Hypertrophied Caudate Lobe, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Marshall University, Huntington, WV; 2Joan C. Edwards School of Medicine, Huntington, WV; 3Marshall University Joan C. Edwards School of Medicine, Huntington, WV
Introduction: Budd‐Chiari syndrome (BCS) is defined as an obstruction of the hepatic venous outflow in the absence of cardiac or pericardial diseases. Obstruction can occur in large hepatic veins, the supra hepatic portion of the inferior vena cava, or small hepatic veins. It is a very rare condition with an incidence below 1 case per million population. The most common clinical presentation of BCS is ascites (83%) and abdominal pain (61%). Inferior vena cava obstruction is seen as the initial symptom. Diagnosis is usually made by demonstration of hepatic venous flow obstruction by noninvasive imaging techniques (Doppler ultrasonography, CT, or MR). However, imaging studies don’t depict BCS in small hepatic veins since images tend not to reveal hepatic venous obstruction leaving liver biopsy and venography as the last line to confirm the diagnosis.
Case Description/Methods: A 51-year-old woman with no significant PMH presented to the emergency department with acute bilateral leg swelling and abdominal swelling for two weeks. She states she is a healthy person. Physical exam: Vital signs: BP: 100/50 mmHg, HR: 110 BPM. Abdominal exam: massive ascites and lower limb swelling with anasarca. The chest exam is clear. She had a normal comprehensive metabolic panel and a normal complete blood count. The abdominal US showed massive ascites. Ascitic fluid studies showed serum ascites fluid gradient of 2.5. with predominantly lymphocytes (95%). Echocardiogram showed a normal ejection fraction of 60% otherwise completely normal. CT abdomen and MR venography showed caudate lobe enlargement compressing IVC with liver parenchymal changes. A tissue biopsy was obtained by endoscopic ultrasound. The patient was found to have Budd Chiari syndrome. Hypercoagulable workup was positive for JAK-2 mutation. The patient was started on Eliquis, Two weeks following the initiation of antithrombotic treatment patient’s abdominal ascites and lower limb swelling started to improve. Right hepatic stent was placed afterward.
Discussion: Budd-Chiari syndrome (BCS) or hepatic vein thrombosis (HVT), is a rare disorder resulting from obstruction of the hepatic venous outflow. It can present as Inferior vena cava obstruction by an enlarged caudate lobe or clot obstructive the IVC lumen. The diagnostic modality of choice is Doppler US, CT, or MRI. Diagnosis can be challenging in small vein hepatic BCS. Biopsy and venography are reserved as last resort to establish the diagnosis.

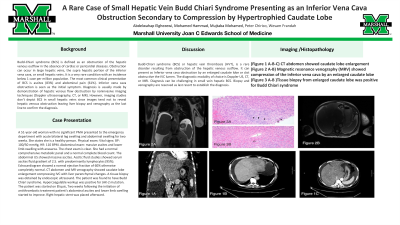
Figure: (Figure 1 A-B-C) CT abdomen showed caudate lobe enlargement
(Figure 2 A-B) Magnetic resonance venography (MRV) showed compression of the inferior vena cava by an enlarged caudate lobe
(Figure 3 A-B )Tissue biopsy from enlarged caudate lobe was positive for Budd Chiari syndrome
(Figure 2 A-B) Magnetic resonance venography (MRV) showed compression of the inferior vena cava by an enlarged caudate lobe
(Figure 3 A-B )Tissue biopsy from enlarged caudate lobe was positive for Budd Chiari syndrome
Disclosures:
Abdelwahap Elghezewi indicated no relevant financial relationships.
Mohamed Hammad indicated no relevant financial relationships.
Mujtaba Mohamed indicated no relevant financial relationships.
Peter Chirico indicated no relevant financial relationships.
Wesam Frandah: Endo gastric solutions – Consultant. Olympus Medical – Consultant.
Abdelwahap Elghezewi, MD1, Mohamed Hammad, MD1, Mujtaba Mohamed, MBBS2, Peter Chirico, MD3, Wesam Frandah, MD3. P1042 - A Rare Case of Small Hepatic Vein Budd Chiari Syndrome Presenting as an Inferior Vena Cava Obstruction Secondary to Compression by Hypertrophied Caudate Lobe, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
