Sunday Poster Session
Category: Liver
P1050 - Ig-Anchoring: A Case of IgA Nephropathy Mistaken for Hepatorenal Syndrome
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Franklyn Wallace, MD
Mayo Clinic
Rochester, MN
Presenting Author(s)
Franklyn Wallace, MD, Maria Gonzalez Suarez, MD, PhD
Mayo Clinic, Rochester, MN
Introduction: While hepatorenal syndrome (HRS) is an important cause of acute kidney injury (AKI) in patients with cirrhosis complicated by ascites, most patients will have an alternative cause for AKI. A diagnosis of HRS requires exclusion of shock, structural kidney injury (via urinalysis and kidney ultrasound), and hypovolemia (via holding diuretics and providing an albumin challenge). Failure to exclude alternative etiologies leads to delayed diagnosis and inappropriate treatment. Our case highlights a rare clinical presentation of a relatively common kidney disease affecting patients with cirrhosis.
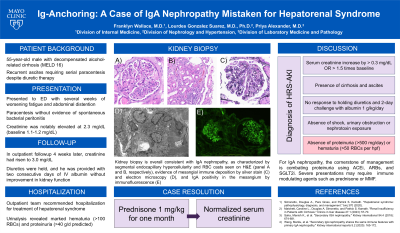
Case Description/Methods: A 49-year-old male with alcohol-related cirrhosis (MELD 16) complicated by recurrent ascites presented to the emergency department with fatigue and abdominal distention. Paracentesis with fluid analysis ruled out spontaneous bacterial peritonitis. Laboratory testing revealed an elevated creatinine at 2.3 mg/dL (baseline 1.1-1.2 mg/dL), which was attributed to hypervolemia with tense ascites. He was dismissed home with plans to resume weekly paracentesis and diuretic titration. Four weeks later, outpatient labs revealed worsened creatinine at 3.0 mg/dL. He discontinued diuretics and received two consecutive days of IV albumin without benefit. He was admitted to the hospital for management of presumed hepatorenal syndrome. On admission, he reported a 2-week history of gross hematuria. A urinalysis revealed marked hematuria and proteinuria. A broad workup was negative for obstruction, thrombotic microangiopathy, glomerular basement membrane disease or vasculitis. A kidney biopsy ultimately revealed IgA nephropathy. He was initiated on prednisone with plans to eventually transition to mycophenolate mofetil.
Discussion: The initial evaluation of patients with AKI should always include thorough history, physical examination, and urinalysis. Identification of hematuria or significant proteinuria in the context of AKI should not be ignored, as they warrant consideration of acute glomerular pathology. Here, we present a case of secondary IgA nephropathy—an underappreciated cause of hematuria and kidney disease in patients with cirrhosis. At the time of liver transplantation, up to 25% of patients have evidence of IgA nephropathy on kidney biopsy, although progression to nephrotic-range proteinuria or rapidly progressive glomerulonephritis is relatively rare. Management includes supportive treatment of proteinuria (ACEi, ARB, and SGLT2i) and immunosuppressive medications in severe cases.
Disclosures:
Franklyn Wallace, MD, Maria Gonzalez Suarez, MD, PhD. P1050 - Ig-Anchoring: A Case of IgA Nephropathy Mistaken for Hepatorenal Syndrome, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Mayo Clinic, Rochester, MN
Introduction: While hepatorenal syndrome (HRS) is an important cause of acute kidney injury (AKI) in patients with cirrhosis complicated by ascites, most patients will have an alternative cause for AKI. A diagnosis of HRS requires exclusion of shock, structural kidney injury (via urinalysis and kidney ultrasound), and hypovolemia (via holding diuretics and providing an albumin challenge). Failure to exclude alternative etiologies leads to delayed diagnosis and inappropriate treatment. Our case highlights a rare clinical presentation of a relatively common kidney disease affecting patients with cirrhosis.
Case Description/Methods: A 49-year-old male with alcohol-related cirrhosis (MELD 16) complicated by recurrent ascites presented to the emergency department with fatigue and abdominal distention. Paracentesis with fluid analysis ruled out spontaneous bacterial peritonitis. Laboratory testing revealed an elevated creatinine at 2.3 mg/dL (baseline 1.1-1.2 mg/dL), which was attributed to hypervolemia with tense ascites. He was dismissed home with plans to resume weekly paracentesis and diuretic titration. Four weeks later, outpatient labs revealed worsened creatinine at 3.0 mg/dL. He discontinued diuretics and received two consecutive days of IV albumin without benefit. He was admitted to the hospital for management of presumed hepatorenal syndrome. On admission, he reported a 2-week history of gross hematuria. A urinalysis revealed marked hematuria and proteinuria. A broad workup was negative for obstruction, thrombotic microangiopathy, glomerular basement membrane disease or vasculitis. A kidney biopsy ultimately revealed IgA nephropathy. He was initiated on prednisone with plans to eventually transition to mycophenolate mofetil.
Discussion: The initial evaluation of patients with AKI should always include thorough history, physical examination, and urinalysis. Identification of hematuria or significant proteinuria in the context of AKI should not be ignored, as they warrant consideration of acute glomerular pathology. Here, we present a case of secondary IgA nephropathy—an underappreciated cause of hematuria and kidney disease in patients with cirrhosis. At the time of liver transplantation, up to 25% of patients have evidence of IgA nephropathy on kidney biopsy, although progression to nephrotic-range proteinuria or rapidly progressive glomerulonephritis is relatively rare. Management includes supportive treatment of proteinuria (ACEi, ARB, and SGLT2i) and immunosuppressive medications in severe cases.
Disclosures:
Franklyn Wallace indicated no relevant financial relationships.
Maria Gonzalez Suarez indicated no relevant financial relationships.
Franklyn Wallace, MD, Maria Gonzalez Suarez, MD, PhD. P1050 - Ig-Anchoring: A Case of IgA Nephropathy Mistaken for Hepatorenal Syndrome, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
