Sunday Poster Session
Category: Liver
P1055 - Clinical Operational Tolerance in Liver Transplant: Are We Making Any Progress?
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio
- GS
Guneet Sidhu, MD
University of North Dakota School of Medicine
Fargo, ND
Presenting Author(s)
Guneet Sidhu, MD1, John T. Bassett, MD2, John Evans, MD3
1University of North Dakota School of Medicine, Fargo, ND; 2Sanford Health, Fargo, ND; 3Sanford Medical Center, Fargo, ND
Introduction: Hereditary tyrosinemia type 1 (HT1), is the most severe disorder of tyrosine metabolism. HT1 occurs in 1 in 12,000 to 1 in 100,000 individuals of Northern European descent. Liver transplantation is an effective treatment.
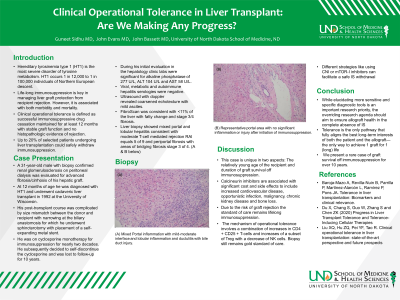
Case Description/Methods: A 31-year-old male with biopsy confirmed renal glomerulosclerosis on peritoneal dialysis was evaluated for advanced fibrosis/cirrhosis of his hepatic graft. At 1 year of age, he was diagnosed with HTI and underwent cadaveric liver transplant in 1992 at the University of Wisconsin at 16 months of age. His post-transplant course was complicated by size mismatch between the donor and recipient with narrowing at the biliary anastomosis for which he underwent sphincterotomy with placement of a self-expanding metal stent. He was on cyclosporine monotherapy for immunosuppression for nearly two decades. He subsequently decided to self-discontinue the cyclosporine and was lost to follow-up for 10 years. During his initial evaluation in the hepatology clinic in April 2022, labs were significant for alkaline phosphatase of 277 U/L, ALT 104 U/L and AST 58 U/L. Viral, metabolic and autoimmune hepatitis serologies were negative. Ultrasound with doppler revealed coarsened echotexture with mild ascites. Liver biopsy showed mixed portal and lobular hepatitis consistent with moderate T-cell mediated Rejection Activity Index (RAI) 5 of 9 and periportal fibrosis with areas of bridging fibrosis stage 3 of 4 (figure 1A). He was treated with Solumedrol 1000 mg IV x 3 d, then oral prednisone. Tacrolimus was started. His liver tests improved and repeat biopsy showed significantly less inflammation, providing no evidence of acute cellular (T cell-mediated) rejection (figure 1B).
Discussion: Calcineurin inhibitors are associated with significant cost and side effects to include increased cardiovascular disease, opportunistic infection, malignancy, chronic kidney disease and bone loss. In a minority of cases, patients achieve operational tolerance (preserved graft function with no immunosuppression). Due to the risk of graft rejection the standard of care remains lifelong immunosuppression. The mechanism of operational tolerance involves a combination of increases in CD4 + CD25 + T-cells and increases of a subset of Treg with a decrease of NK cells. Studies are ongoing to identify biomarkers of operational tolerance as well as predictors of acute rejection. We present a rare case of graft survival off immunosuppression for over 10 years.

Disclosures:
Guneet Sidhu, MD1, John T. Bassett, MD2, John Evans, MD3. P1055 - Clinical Operational Tolerance in Liver Transplant: Are We Making Any Progress?, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of North Dakota School of Medicine, Fargo, ND; 2Sanford Health, Fargo, ND; 3Sanford Medical Center, Fargo, ND
Introduction: Hereditary tyrosinemia type 1 (HT1), is the most severe disorder of tyrosine metabolism. HT1 occurs in 1 in 12,000 to 1 in 100,000 individuals of Northern European descent. Liver transplantation is an effective treatment.
Case Description/Methods: A 31-year-old male with biopsy confirmed renal glomerulosclerosis on peritoneal dialysis was evaluated for advanced fibrosis/cirrhosis of his hepatic graft. At 1 year of age, he was diagnosed with HTI and underwent cadaveric liver transplant in 1992 at the University of Wisconsin at 16 months of age. His post-transplant course was complicated by size mismatch between the donor and recipient with narrowing at the biliary anastomosis for which he underwent sphincterotomy with placement of a self-expanding metal stent. He was on cyclosporine monotherapy for immunosuppression for nearly two decades. He subsequently decided to self-discontinue the cyclosporine and was lost to follow-up for 10 years. During his initial evaluation in the hepatology clinic in April 2022, labs were significant for alkaline phosphatase of 277 U/L, ALT 104 U/L and AST 58 U/L. Viral, metabolic and autoimmune hepatitis serologies were negative. Ultrasound with doppler revealed coarsened echotexture with mild ascites. Liver biopsy showed mixed portal and lobular hepatitis consistent with moderate T-cell mediated Rejection Activity Index (RAI) 5 of 9 and periportal fibrosis with areas of bridging fibrosis stage 3 of 4 (figure 1A). He was treated with Solumedrol 1000 mg IV x 3 d, then oral prednisone. Tacrolimus was started. His liver tests improved and repeat biopsy showed significantly less inflammation, providing no evidence of acute cellular (T cell-mediated) rejection (figure 1B).
Discussion: Calcineurin inhibitors are associated with significant cost and side effects to include increased cardiovascular disease, opportunistic infection, malignancy, chronic kidney disease and bone loss. In a minority of cases, patients achieve operational tolerance (preserved graft function with no immunosuppression). Due to the risk of graft rejection the standard of care remains lifelong immunosuppression. The mechanism of operational tolerance involves a combination of increases in CD4 + CD25 + T-cells and increases of a subset of Treg with a decrease of NK cells. Studies are ongoing to identify biomarkers of operational tolerance as well as predictors of acute rejection. We present a rare case of graft survival off immunosuppression for over 10 years.

Figure: (A) Mixed Portal inflammation with mild-moderate interface and lobular inflammation and ductulitis with bile duct injury
(B) Representative portal area with no significant inflammation or injury after initiation of immunosuppression
(B) Representative portal area with no significant inflammation or injury after initiation of immunosuppression
Disclosures:
Guneet Sidhu indicated no relevant financial relationships.
John Bassett indicated no relevant financial relationships.
John Evans indicated no relevant financial relationships.
Guneet Sidhu, MD1, John T. Bassett, MD2, John Evans, MD3. P1055 - Clinical Operational Tolerance in Liver Transplant: Are We Making Any Progress?, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
