Sunday Poster Session
Category: Liver
P1057 - Multiple Hepatic Lesions With Portal Vein Thrombosis: Abscesses or Metastatic Malignancy?
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Alejandro J. Loyola-Velez, MD
VA Caribbean Healthcare System
Isabela, PR
Presenting Author(s)
Alejandro J.. Loyola-Velez, MD1, Carla M. Cepero-Jimenez, MD2, Marilee Tiru-Vega, MD2, Pedro Rosa-Cortes, MD2, Jose Martin-Ortiz, MD, FACG2, Doris H. Toro, MD, FACG2
1VA Caribbean Healthcare System, Isabela, Puerto Rico; 2VA Caribbean Healthcare System, San Juan, Puerto Rico
Introduction: Hepatic abscesses (HA) are rare, and incidence varies between regions, but mortality has been estimated to reach up to 15%. In early stages, HA can be difficult to distinguish from malignancy by appearing centrally hypodense with peripheral enhancement on imaging, requiring a clinically holistic approach for diagnosis. Management entails drainage, often sono-guided. However, classifying the source of infection is crucial to achieve resolution and avoid recurrence. Underlying biliary tract disease is known to be responsible for as much as 50% of HA. When associated to choledocholithiasis, ERCP prior to percutaneous drainage is indicated for source control of infection. We present the case of a patient with non-specific symptoms and multiple hepatic lesions on imaging, identified to be pyogenic abscesses secondary to choledocholithiasis.
Case Description/Methods: This is the case of an 86-year-old male who arrived at the emergency department for evaluation of anorexia and weakness. The patient had tachycardia and leukocytosis in laboratories. Physical exam revealed a benign abdomen. Abdominopelvic CT with IV contrast revealed multiple hypodense lesions (largest measuring 4cm) with peripheral enhancement, suggestive of abscesses versus malignancy, left portal vein thrombosis, a dilated common bile duct and choledocholithiasis. Empiric antibiotic therapy and full-dose anticoagulation was initiated. An ERCP was performed, with successful stone removal. HA were subsequently drained via sonographic-guidance. Aspirate was positive for E. faecalis. The patient had marked clinical improvement and completed a 21-day regimen of antibiotics with resolution of HA.
Discussion: Radiographic imaging provides an excellent advantage in the diagnosis of intra-abdominal pathology, but critical thinking remains crucial in distinguishing between diagnoses with similar presentation. Our patient presented with a smoldering infection with signs and symptoms suggestive of malignancy. Although, portal vein thrombosis (PVT) in a healthy liver is usually associated with a prothrombotic state; in our case, it was determined to be secondary to pylephlebitis. The latter is an uncommon cause of PVT which can result in intrabdominal/pelvic sepsis of varied etiology. Identification of an infectious biliary process that could explain the patient’s lesions as abscesses and the cause of the portal vein thrombosis allowed for prompt management of a pathology with significant morbidity and mortality.

Disclosures:
Alejandro J.. Loyola-Velez, MD1, Carla M. Cepero-Jimenez, MD2, Marilee Tiru-Vega, MD2, Pedro Rosa-Cortes, MD2, Jose Martin-Ortiz, MD, FACG2, Doris H. Toro, MD, FACG2. P1057 - Multiple Hepatic Lesions With Portal Vein Thrombosis: Abscesses or Metastatic Malignancy?, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1VA Caribbean Healthcare System, Isabela, Puerto Rico; 2VA Caribbean Healthcare System, San Juan, Puerto Rico
Introduction: Hepatic abscesses (HA) are rare, and incidence varies between regions, but mortality has been estimated to reach up to 15%. In early stages, HA can be difficult to distinguish from malignancy by appearing centrally hypodense with peripheral enhancement on imaging, requiring a clinically holistic approach for diagnosis. Management entails drainage, often sono-guided. However, classifying the source of infection is crucial to achieve resolution and avoid recurrence. Underlying biliary tract disease is known to be responsible for as much as 50% of HA. When associated to choledocholithiasis, ERCP prior to percutaneous drainage is indicated for source control of infection. We present the case of a patient with non-specific symptoms and multiple hepatic lesions on imaging, identified to be pyogenic abscesses secondary to choledocholithiasis.
Case Description/Methods: This is the case of an 86-year-old male who arrived at the emergency department for evaluation of anorexia and weakness. The patient had tachycardia and leukocytosis in laboratories. Physical exam revealed a benign abdomen. Abdominopelvic CT with IV contrast revealed multiple hypodense lesions (largest measuring 4cm) with peripheral enhancement, suggestive of abscesses versus malignancy, left portal vein thrombosis, a dilated common bile duct and choledocholithiasis. Empiric antibiotic therapy and full-dose anticoagulation was initiated. An ERCP was performed, with successful stone removal. HA were subsequently drained via sonographic-guidance. Aspirate was positive for E. faecalis. The patient had marked clinical improvement and completed a 21-day regimen of antibiotics with resolution of HA.
Discussion: Radiographic imaging provides an excellent advantage in the diagnosis of intra-abdominal pathology, but critical thinking remains crucial in distinguishing between diagnoses with similar presentation. Our patient presented with a smoldering infection with signs and symptoms suggestive of malignancy. Although, portal vein thrombosis (PVT) in a healthy liver is usually associated with a prothrombotic state; in our case, it was determined to be secondary to pylephlebitis. The latter is an uncommon cause of PVT which can result in intrabdominal/pelvic sepsis of varied etiology. Identification of an infectious biliary process that could explain the patient’s lesions as abscesses and the cause of the portal vein thrombosis allowed for prompt management of a pathology with significant morbidity and mortality.

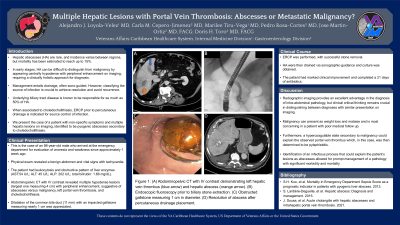
Figure: (A) Abdominopelvic CT with IV contrast demonstrating left hepatic vein thrombus (blue arrow) and hepatic abscess (orange arrow). (B) Endoscopic fluoroscopy prior to biliary stone extraction. (C) Obstructed gallstone measuring 1 cm in diameter. (D) Resolution of abscess after percutaneous drainage placement.
Disclosures:
Alejandro Loyola-Velez indicated no relevant financial relationships.
Carla Cepero-Jimenez indicated no relevant financial relationships.
Marilee Tiru-Vega indicated no relevant financial relationships.
Pedro Rosa-Cortes indicated no relevant financial relationships.
Jose Martin-Ortiz indicated no relevant financial relationships.
Doris Toro indicated no relevant financial relationships.
Alejandro J.. Loyola-Velez, MD1, Carla M. Cepero-Jimenez, MD2, Marilee Tiru-Vega, MD2, Pedro Rosa-Cortes, MD2, Jose Martin-Ortiz, MD, FACG2, Doris H. Toro, MD, FACG2. P1057 - Multiple Hepatic Lesions With Portal Vein Thrombosis: Abscesses or Metastatic Malignancy?, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
