Sunday Poster Session
Category: Liver
P1062 - An Unfamiliar Case of Pyogenic Liver Abscess: Hepatic Actinomycosis
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio
.jpg)
Jiteshwar S. Pannu, MD
University of Oklahoma Health Sciences Center
Oklahoma City, OK
Presenting Author(s)
Jiteshwar S. Pannu, MD, Steven M. Harsha, MD, Salar Faiazi, MD
University of Oklahoma Health Sciences Center, Oklahoma City, OK
Introduction: Abdominopelvic actinomycosis may manifest as rectal/anal infections, abscesses or IUD related pelvic infections. Hepatic actinomycosis (HA) is a rare disorder and given its vague clinical presentation, diagnosis is tricky and often necessitates microbiological/pathological confirmation. Herein, we highlight a patient diagnosed with HA in the setting of recent perforated peptic ulcer, managed with antibiotics and percutaneous drainage.
Case Description/Methods: 72-year-old female with a history of recent abdominal surgery for peritonitis secondary to a perforated peptic ulcer, was admitted with complaints of nausea, confusion and diffuse abdominal pain. Physical exam was remarkable for poor dentition, diffusely tender abdomen with an intact laparotomy scar. Laboratory evaluation revealed leukocytosis and elevated transaminases. CT abdomen revealed a 8.7 X 5.1 X 3.1 cm multi-lobulated peripherally enhancing gas containing fluid collection. Given the CT findings suggestive of a pyogenic liver abscess, a percutaneous (PC) drainage was performed, draining 200 cc of greenish purulent fluid, with placement of a 14 Fr biliary drain. Abscess fluid culture grew actinomyces odontolyticus. The patient was continued on intravenous (IV) piperacillin tazobactam and a repeat CT scan done 1 week later revealed near resolution of the abscess. As a result, the drain was removed, and the patient was discharged home to complete 4 weeks of IV antibiotics followed by 12 months of suppressive oral amoxicillin. She was also referred for a dental appointment to address dental caries.
Discussion: Actinomyces spp. normally colonizes the gastrointestinal and female reproductive tract. Predisposing factors for HA include an underlying mucosal breach such as poor dentition, peptic ulcer and recent abdominal surgery. On cross sectional imaging, it may be misinterpreted as malignancy, hydatid cyst etc., hence diagnosis requires microbiological confirmation revealing gram positive filamentous bacteria. Treatment modalities include source control via surgical/PC drainage or hepatic resection and appropriate antibiotics such as amoxicillin and higher penicillin derivatives, fluoroquinolones, doxycycline and aztreonam. If left untreated, it can potentially cause life-threatening complications such as sepsis, disseminated actinomycosis and coagulopathy. It is also prudent to address the underlying predisposing factors for systemic actinomycosis, such as poor dentition and recent peptic ulcer perforation in our patient.

Disclosures:
Jiteshwar S. Pannu, MD, Steven M. Harsha, MD, Salar Faiazi, MD. P1062 - An Unfamiliar Case of Pyogenic Liver Abscess: Hepatic Actinomycosis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
University of Oklahoma Health Sciences Center, Oklahoma City, OK
Introduction: Abdominopelvic actinomycosis may manifest as rectal/anal infections, abscesses or IUD related pelvic infections. Hepatic actinomycosis (HA) is a rare disorder and given its vague clinical presentation, diagnosis is tricky and often necessitates microbiological/pathological confirmation. Herein, we highlight a patient diagnosed with HA in the setting of recent perforated peptic ulcer, managed with antibiotics and percutaneous drainage.
Case Description/Methods: 72-year-old female with a history of recent abdominal surgery for peritonitis secondary to a perforated peptic ulcer, was admitted with complaints of nausea, confusion and diffuse abdominal pain. Physical exam was remarkable for poor dentition, diffusely tender abdomen with an intact laparotomy scar. Laboratory evaluation revealed leukocytosis and elevated transaminases. CT abdomen revealed a 8.7 X 5.1 X 3.1 cm multi-lobulated peripherally enhancing gas containing fluid collection. Given the CT findings suggestive of a pyogenic liver abscess, a percutaneous (PC) drainage was performed, draining 200 cc of greenish purulent fluid, with placement of a 14 Fr biliary drain. Abscess fluid culture grew actinomyces odontolyticus. The patient was continued on intravenous (IV) piperacillin tazobactam and a repeat CT scan done 1 week later revealed near resolution of the abscess. As a result, the drain was removed, and the patient was discharged home to complete 4 weeks of IV antibiotics followed by 12 months of suppressive oral amoxicillin. She was also referred for a dental appointment to address dental caries.
Discussion: Actinomyces spp. normally colonizes the gastrointestinal and female reproductive tract. Predisposing factors for HA include an underlying mucosal breach such as poor dentition, peptic ulcer and recent abdominal surgery. On cross sectional imaging, it may be misinterpreted as malignancy, hydatid cyst etc., hence diagnosis requires microbiological confirmation revealing gram positive filamentous bacteria. Treatment modalities include source control via surgical/PC drainage or hepatic resection and appropriate antibiotics such as amoxicillin and higher penicillin derivatives, fluoroquinolones, doxycycline and aztreonam. If left untreated, it can potentially cause life-threatening complications such as sepsis, disseminated actinomycosis and coagulopathy. It is also prudent to address the underlying predisposing factors for systemic actinomycosis, such as poor dentition and recent peptic ulcer perforation in our patient.

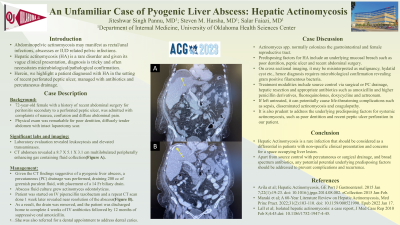
Figure: Figure A: CT abdomen revealing a 8.7 X 5.1 X 3.1 cm multilobulated peripherally enhancing gas containing fluid collection (yellow arrow) concerning for pyogenic liver abscess;
Figure B: Repeat CT abdomen 1 week post percutaneous drainage showing near resolution of the abscess with the 14 Fr percutaneous drain in place (yellow arrow)
Figure B: Repeat CT abdomen 1 week post percutaneous drainage showing near resolution of the abscess with the 14 Fr percutaneous drain in place (yellow arrow)
Disclosures:
Jiteshwar Pannu indicated no relevant financial relationships.
Steven Harsha indicated no relevant financial relationships.
Salar Faiazi indicated no relevant financial relationships.
Jiteshwar S. Pannu, MD, Steven M. Harsha, MD, Salar Faiazi, MD. P1062 - An Unfamiliar Case of Pyogenic Liver Abscess: Hepatic Actinomycosis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
