Sunday Poster Session
Category: Liver
P1066 - Rejected! A Case of Steroid-Resistant Acute Cellular Rejection Following Living Donor Liver Transplantation
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Anastasia Naritsin, DO
Lahey Hospital and Medical Center
Woburn, MA
Presenting Author(s)
Anastasia Naritsin, DO1, Umnia Shnawa, MD2, Ahlam Alzoghoul, MD2, Mohammad Almeqdadi, MD3
1Lahey Hospital and Medical Center, Burlington, MA; 2Jordan University of Science and Technology, Irbid, Irbid, Jordan; 3Lahey Hospital, Burlington, MA
Introduction: Acute cellular rejection (ACR), typically treated with steroid pulse therapy is a common complication following liver transplantation, occurring in approximately 15-25% of patients. Steroid-resistant ACR (SRACR) is less common, occurring in approximately 10% of ACR cases, and is associated with increased morbidity and mortality. This case describes the management of SRACR in a 58-year-old male with decompensated cirrhosis secondary to nonalcoholic steatohepatitis (NASH) following living donor liver transplantation (LDLT).
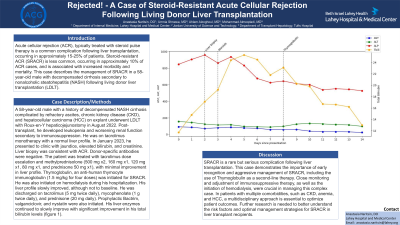
Case Description/Methods: A 58-year-old male with a history of decompensated NASH cirrhosis complicated by refractory ascites, chronic kidney disease (CKD), and hepatocellular carcinoma (HCC) on explant underwent LDLT with Roux-en-Y hepaticojejunostomy in August 2022. Post-transplant, he developed leukopenia and worsening renal function secondary to immunosuppression. He was on tacrolimus monotherapy with a normal liver profile. In January 2023, he presented to clinic with jaundice, elevated bilirubin, and creatinine. Liver biopsy was consistent with ACR. Donor-specific antibodies were negative. The patient was treated with tacrolimus dose escalation and methylprednisolone (500 mg x2, 160 mg x1, 120 mg x1, 80 mg x1, and prednisone 50 mg x1), with minimal improvement in liver profile. Thymoglobulin, an anti-human thymocyte immunoglobulin (1.5 mg/kg for four doses) was initiated for SRACR. He was also initiated on hemodialysis during his hospitalization. His liver profile slowly improved, although not to baseline. He was discharged on tacrolimus (5 mg twice daily), mycophenolate (1 g twice daily), and prednisone (20 mg daily). Prophylactic Bactrim, valganciclovir, and nystatin were also initiated. His liver enzymes continued to slowly improve with significant improvement in his total bilirubin levels (figure 1).
Discussion: SRACR is a rare but serious complication following liver transplantation. This case demonstrates the importance of early recognition and aggressive management of SRACR, including the use of Thymoglobulin as a second-line therapy. Close monitoring and adjustment of immunosuppressive therapy, as well as the initiation of hemodialysis, were crucial in managing this complex case. In patients with multiple comorbidities, such as CKD, anemia, and HCC, a multidisciplinary approach is essential to optimize patient outcomes. Further research is needed to better understand the risk factors and optimal management strategies for SRACR in liver transplant recipients.

Disclosures:
Anastasia Naritsin, DO1, Umnia Shnawa, MD2, Ahlam Alzoghoul, MD2, Mohammad Almeqdadi, MD3. P1066 - Rejected! A Case of Steroid-Resistant Acute Cellular Rejection Following Living Donor Liver Transplantation, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Lahey Hospital and Medical Center, Burlington, MA; 2Jordan University of Science and Technology, Irbid, Irbid, Jordan; 3Lahey Hospital, Burlington, MA
Introduction: Acute cellular rejection (ACR), typically treated with steroid pulse therapy is a common complication following liver transplantation, occurring in approximately 15-25% of patients. Steroid-resistant ACR (SRACR) is less common, occurring in approximately 10% of ACR cases, and is associated with increased morbidity and mortality. This case describes the management of SRACR in a 58-year-old male with decompensated cirrhosis secondary to nonalcoholic steatohepatitis (NASH) following living donor liver transplantation (LDLT).
Case Description/Methods: A 58-year-old male with a history of decompensated NASH cirrhosis complicated by refractory ascites, chronic kidney disease (CKD), and hepatocellular carcinoma (HCC) on explant underwent LDLT with Roux-en-Y hepaticojejunostomy in August 2022. Post-transplant, he developed leukopenia and worsening renal function secondary to immunosuppression. He was on tacrolimus monotherapy with a normal liver profile. In January 2023, he presented to clinic with jaundice, elevated bilirubin, and creatinine. Liver biopsy was consistent with ACR. Donor-specific antibodies were negative. The patient was treated with tacrolimus dose escalation and methylprednisolone (500 mg x2, 160 mg x1, 120 mg x1, 80 mg x1, and prednisone 50 mg x1), with minimal improvement in liver profile. Thymoglobulin, an anti-human thymocyte immunoglobulin (1.5 mg/kg for four doses) was initiated for SRACR. He was also initiated on hemodialysis during his hospitalization. His liver profile slowly improved, although not to baseline. He was discharged on tacrolimus (5 mg twice daily), mycophenolate (1 g twice daily), and prednisone (20 mg daily). Prophylactic Bactrim, valganciclovir, and nystatin were also initiated. His liver enzymes continued to slowly improve with significant improvement in his total bilirubin levels (figure 1).
Discussion: SRACR is a rare but serious complication following liver transplantation. This case demonstrates the importance of early recognition and aggressive management of SRACR, including the use of Thymoglobulin as a second-line therapy. Close monitoring and adjustment of immunosuppressive therapy, as well as the initiation of hemodialysis, were crucial in managing this complex case. In patients with multiple comorbidities, such as CKD, anemia, and HCC, a multidisciplinary approach is essential to optimize patient outcomes. Further research is needed to better understand the risk factors and optimal management strategies for SRACR in liver transplant recipients.

Figure: Title: Laboratory Markers Pre- and Post-Thymoglobulin Treatment for Steroid Resistant Acute Cellular Rejection
Disclosures:
Anastasia Naritsin indicated no relevant financial relationships.
Umnia Shnawa indicated no relevant financial relationships.
Ahlam Alzoghoul indicated no relevant financial relationships.
Mohammad Almeqdadi indicated no relevant financial relationships.
Anastasia Naritsin, DO1, Umnia Shnawa, MD2, Ahlam Alzoghoul, MD2, Mohammad Almeqdadi, MD3. P1066 - Rejected! A Case of Steroid-Resistant Acute Cellular Rejection Following Living Donor Liver Transplantation, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
