Sunday Poster Session
Category: Liver
P1071 - When it’s Not Cirrhosis: A Case of Portal Hypertension After Neonatal Instrumentation
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Colleen Boyle, MD
Naval Medical Center
San Diego, CA
Presenting Author(s)
Award: Presidential Poster Award
Jeffrey Allison, MD1, Colleen Boyle, MD1, Brett Sadowski, MD2
1Naval Medical Center, Portsmouth, VA; 2Naval Medical Center, San Diego, CA
Introduction: Portal venous hypertension (PVH) can induce life-threatening gastrointestinal bleeding and is most often a consequence of liver cirrhosis, although a spectrum of etiologies has been identified. There is a growing body of literature examining iatrogenic causes, particularly umbilical vein central access, known to cause thrombotic portal vein disease in neonates and PVH during childhood. Here we present a case of an adult female with non-cirrhotic PVH and variceal bleeding later discovered to have undergone vascular manipulation in early infancy.
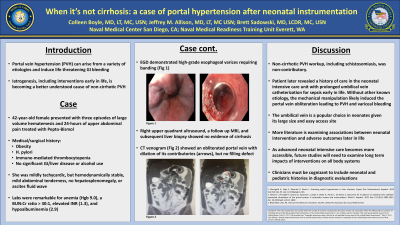
Case Description/Methods: A 42-year-old female with thrombocytopenia previously attributed to a prior Helicobacter pylori infection with associated immune-mediated thrombocytopenia, presented with acute onset large volume hematemesis after 24 hours of abdominal discomfort. She had no known history of chronic liver disease or common risk factors for cirrhosis. She was tachycardic, with mild epigastric tenderness and splenomegaly. Labs notable for anemia, thrombocytopenia, BUN:Cr >30:1, elevated INR, and hypoalbuminemia. She was resuscitated with blood products and admitted to the step-down unit for further monitoring. Upper endoscopy demonstrated stigmata of PVH including recent bleeding from esophageal varices which were banded. CT abdomen and pelvis showed multiple large esophageal varices and splenomegaly but a normal liver. MRI liver noted diminished portal venous flow initially thought to be thrombosis; however, CT venogram revealed an obliterated portal vein with no thrombosis, along with severe periesophageal varices, peri-splenic and peripancreatic vascular congestion. Upon further questioning she disclosed that she had a prolonged neonatal intensive care unit stay for sepsis with umbilical vein catheterization. She was placed on a non-selective beta blocker and had surveillance endoscopy, without further bleeding.
Discussion: Patient’s PVH was presumed to be related to prolonged umbilical vein catheterization leading to eventual obliteration of the portal vein and variceal hemorrhage. Supportive details include chronic thrombocytopenia, splenomegaly, and degree of collateralization. This is consistent with new literature suggesting a link between perinatal umbilical vein interventions and subsequent portal-hepatic complications. As the incidence of such interventions grows, future studies will need to examine their long-term impacts, and clinicians will need to include perinatal hospitalization/interventions in their diagnostic evaluation.

Disclosures:
Jeffrey Allison, MD1, Colleen Boyle, MD1, Brett Sadowski, MD2. P1071 - When it’s Not Cirrhosis: A Case of Portal Hypertension After Neonatal Instrumentation, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Jeffrey Allison, MD1, Colleen Boyle, MD1, Brett Sadowski, MD2
1Naval Medical Center, Portsmouth, VA; 2Naval Medical Center, San Diego, CA
Introduction: Portal venous hypertension (PVH) can induce life-threatening gastrointestinal bleeding and is most often a consequence of liver cirrhosis, although a spectrum of etiologies has been identified. There is a growing body of literature examining iatrogenic causes, particularly umbilical vein central access, known to cause thrombotic portal vein disease in neonates and PVH during childhood. Here we present a case of an adult female with non-cirrhotic PVH and variceal bleeding later discovered to have undergone vascular manipulation in early infancy.
Case Description/Methods: A 42-year-old female with thrombocytopenia previously attributed to a prior Helicobacter pylori infection with associated immune-mediated thrombocytopenia, presented with acute onset large volume hematemesis after 24 hours of abdominal discomfort. She had no known history of chronic liver disease or common risk factors for cirrhosis. She was tachycardic, with mild epigastric tenderness and splenomegaly. Labs notable for anemia, thrombocytopenia, BUN:Cr >30:1, elevated INR, and hypoalbuminemia. She was resuscitated with blood products and admitted to the step-down unit for further monitoring. Upper endoscopy demonstrated stigmata of PVH including recent bleeding from esophageal varices which were banded. CT abdomen and pelvis showed multiple large esophageal varices and splenomegaly but a normal liver. MRI liver noted diminished portal venous flow initially thought to be thrombosis; however, CT venogram revealed an obliterated portal vein with no thrombosis, along with severe periesophageal varices, peri-splenic and peripancreatic vascular congestion. Upon further questioning she disclosed that she had a prolonged neonatal intensive care unit stay for sepsis with umbilical vein catheterization. She was placed on a non-selective beta blocker and had surveillance endoscopy, without further bleeding.
Discussion: Patient’s PVH was presumed to be related to prolonged umbilical vein catheterization leading to eventual obliteration of the portal vein and variceal hemorrhage. Supportive details include chronic thrombocytopenia, splenomegaly, and degree of collateralization. This is consistent with new literature suggesting a link between perinatal umbilical vein interventions and subsequent portal-hepatic complications. As the incidence of such interventions grows, future studies will need to examine their long-term impacts, and clinicians will need to include perinatal hospitalization/interventions in their diagnostic evaluation.

Figure: Image 1: Portal venous obliteration
Disclosures:
Jeffrey Allison indicated no relevant financial relationships.
Colleen Boyle indicated no relevant financial relationships.
Brett Sadowski indicated no relevant financial relationships.
Jeffrey Allison, MD1, Colleen Boyle, MD1, Brett Sadowski, MD2. P1071 - When it’s Not Cirrhosis: A Case of Portal Hypertension After Neonatal Instrumentation, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

