Sunday Poster Session
Category: Liver
P1073 - Infiltrative Peripheral T-Cell Lymphoma: A Rare Cause of Acute Liver Failure
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio
- EK
Elias Kovoor
University of Iowa
Iowa City, IA
Presenting Author(s)
Elias Kovoor, 1, Louma Rustam, MD1, Mary Stone, MD1, Brady Evans, MD1, Randhir Jesudoss, MD2, Kyle Brown, MD3
1University of Iowa, Iowa City, IA; 2Bayfront Health Digestive Health Institute, St. Petersburg, FL; 3University of Iowa Hospitals & Clinics, Iowa City, IA
Introduction: Acute liver failure (ALF) affects ~2000 individuals annually in the United States. ALF due to malignancy accounts for 1.4% of cases and 0.16% are due to T-cell lymphomas. ALF due to malignant infiltration is associated with a mortality of 85% within 3 weeks.
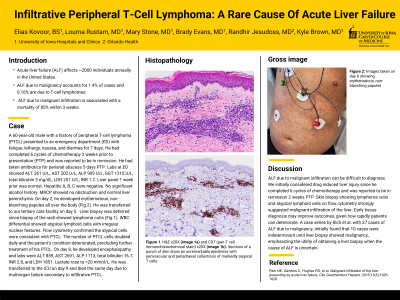
Case Description/Methods: A 60-year-old male with a history of peripheral T-cell lymphoma (PTCL) presented to an emergency department (ED) with fatigue, lethargy, nausea, and diarrhea for 7 days. He had completed 6 cycles of chemotherapy 2 weeks prior to presentation (PTP) and was reported to be in remission. He had taken antibiotics for perianal abscess 5 days PTP. Labs at ED showed ALT 261 U/L, AST 202 U/L, ALP 909 U/L, GGT 1215 U/L, total bilirubin 3 mg/dL, LDH 251 U/L, INR 1.2. Liver panel 1 week prior was normal. Hepatitis A, B, C were negative. No significant alcohol history. MRCP showed no obstruction and normal liver parenchyma. On day 2, he developed erythematous, non-blanching papules all over the body (Fig 1). He was transferred to our tertiary care facility on day 5. Liver biopsy was deferred since biopsy of the rash showed lymphoma cutis (Fig 2). WBC differential showed atypical lymphoid cells with irregular nuclear features. Flow cytometry confirmed the atypical cells were consistent with PTCL. The number of PTCL cells doubled daily and the patient’s condition deteriorated, precluding further treatment of his PTCL. On day 8, he developed encephalopathy and labs were ALT 859, AST 2691, ALP 1113, total bilirubin 16.7, INR 2.8, and LDH 1851. Lactate rose to >20 mmol/L. He was transferred to the ICU on day 9 and died the same day due to multiorgan failure secondary to infiltrative PTCL.
Discussion: ALF due to malignant infiltration can be difficult to diagnose. We initially considered drug induced liver injury since he completed 6 cycles of chemotherapy and was reported to be in remission 2 weeks PTP. Skin biopsy showing lymphoma cutis and atypical lymphoid cells on flow cytometry strongly suggested malignant infiltration of the liver. Early tissue diagnosis may improve outcomes, given how rapidly patients can deteriorate. A case series by Rich et al. with 27 cases of ALF due to malignancy, initially found that 10 cases were indeterminant until liver biopsy showed malignancy, emphasizing the utility of obtaining a liver biopsy when the cause of ALF is uncertain.
Reference:
Rich NE, Sanders C, Hughes RS, et al. Malignant infiltration of the liver presenting as acute liver failure. Clin Gastroenterol Hepatol. 2015;13(5):1025-1028.

Disclosures:
Elias Kovoor, 1, Louma Rustam, MD1, Mary Stone, MD1, Brady Evans, MD1, Randhir Jesudoss, MD2, Kyle Brown, MD3. P1073 - Infiltrative Peripheral T-Cell Lymphoma: A Rare Cause of Acute Liver Failure, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Iowa, Iowa City, IA; 2Bayfront Health Digestive Health Institute, St. Petersburg, FL; 3University of Iowa Hospitals & Clinics, Iowa City, IA
Introduction: Acute liver failure (ALF) affects ~2000 individuals annually in the United States. ALF due to malignancy accounts for 1.4% of cases and 0.16% are due to T-cell lymphomas. ALF due to malignant infiltration is associated with a mortality of 85% within 3 weeks.
Case Description/Methods: A 60-year-old male with a history of peripheral T-cell lymphoma (PTCL) presented to an emergency department (ED) with fatigue, lethargy, nausea, and diarrhea for 7 days. He had completed 6 cycles of chemotherapy 2 weeks prior to presentation (PTP) and was reported to be in remission. He had taken antibiotics for perianal abscess 5 days PTP. Labs at ED showed ALT 261 U/L, AST 202 U/L, ALP 909 U/L, GGT 1215 U/L, total bilirubin 3 mg/dL, LDH 251 U/L, INR 1.2. Liver panel 1 week prior was normal. Hepatitis A, B, C were negative. No significant alcohol history. MRCP showed no obstruction and normal liver parenchyma. On day 2, he developed erythematous, non-blanching papules all over the body (Fig 1). He was transferred to our tertiary care facility on day 5. Liver biopsy was deferred since biopsy of the rash showed lymphoma cutis (Fig 2). WBC differential showed atypical lymphoid cells with irregular nuclear features. Flow cytometry confirmed the atypical cells were consistent with PTCL. The number of PTCL cells doubled daily and the patient’s condition deteriorated, precluding further treatment of his PTCL. On day 8, he developed encephalopathy and labs were ALT 859, AST 2691, ALP 1113, total bilirubin 16.7, INR 2.8, and LDH 1851. Lactate rose to >20 mmol/L. He was transferred to the ICU on day 9 and died the same day due to multiorgan failure secondary to infiltrative PTCL.
Discussion: ALF due to malignant infiltration can be difficult to diagnose. We initially considered drug induced liver injury since he completed 6 cycles of chemotherapy and was reported to be in remission 2 weeks PTP. Skin biopsy showing lymphoma cutis and atypical lymphoid cells on flow cytometry strongly suggested malignant infiltration of the liver. Early tissue diagnosis may improve outcomes, given how rapidly patients can deteriorate. A case series by Rich et al. with 27 cases of ALF due to malignancy, initially found that 10 cases were indeterminant until liver biopsy showed malignancy, emphasizing the utility of obtaining a liver biopsy when the cause of ALF is uncertain.
Reference:
Rich NE, Sanders C, Hughes RS, et al. Malignant infiltration of the liver presenting as acute liver failure. Clin Gastroenterol Hepatol. 2015;13(5):1025-1028.

Figure: Figure 1: Image taken on day 6 showing erythematous, non-blanching papules. Figure 2: H&E x20X (image 2a) and CD7 (pan-T cell immunohistochemical stain) x20X (image 2b). Sections of a punch of skin show an unremarkable epidermis with perivascular and periadnexal collections of markedly atypical T cells.
Disclosures:
Elias Kovoor indicated no relevant financial relationships.
Louma Rustam indicated no relevant financial relationships.
Mary Stone indicated no relevant financial relationships.
Brady Evans indicated no relevant financial relationships.
Randhir Jesudoss indicated no relevant financial relationships.
Kyle Brown indicated no relevant financial relationships.
Elias Kovoor, 1, Louma Rustam, MD1, Mary Stone, MD1, Brady Evans, MD1, Randhir Jesudoss, MD2, Kyle Brown, MD3. P1073 - Infiltrative Peripheral T-Cell Lymphoma: A Rare Cause of Acute Liver Failure, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
