Sunday Poster Session
Category: Liver
P1081 - Lodged in the Liver: A Case of Foreign Body Granulomatosis From Injection Drug Use
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio
- DA
Daniel J. Alvarez, MD
Montefiore Medical Center/Albert Einstein College of Medicine
Bronx, NY
Presenting Author(s)
Daniel J. Alvarez, MD, Alexander Abadir, MD, Geetika Goyal, MD, Kristina Chacko, MD
Montefiore Medical Center/Albert Einstein College of Medicine, Bronx, NY
Introduction: Granulomatosis as a foreign body reaction has been described in the setting of prosthesis placement, cosmetic procedures, retained surgical debris, and injection drug use. Most commonly, granulomas involve the skin and soft tissues but may also affect the lung, liver, arachnoid membrane or occur as a systemic granulomatous reaction with multi-organ involvement. Additives such as talc have been implicated as the cause.
Case Description/Methods: The patient is a 46 year-old female who initially presented with worsening nausea, vomiting, epigastric pain, anorexia and weight loss for 2 months. Her medical history was notable for active injection drug use with opioids. Initial labs were remarkable for pancytopenia: white blood cells 2.3k/uL, hemoglobin 9.5g/dL, and platelets 47k/uL. Liver tests were notable for a cholestatic pattern with alkaline phosphatase of 2061U/L, AST of 144U/L, ALT of 70U/L, total bilirubin of 1.4, and albumin of 2.9g/dL. A gamma-glutamyl transferase was 845U/L. An extensive laboratory evaluation for autoimmune and infectious etiologies was negative. Copper levels and ceruloplasmin were normal. Abdominal imaging including CT and MRI showed hepatosplenomegaly and lymphadenopathy. Chest x-ray revealed no hilar lymphadenopathy and she had no respiratory symptoms. Transfemoral hepatic biopsy was performed. Pathology showed portal tracts with moderate lymphocytic inflammation and non-necrotizing giant cell granulomas surrounded by a lymphoid cuff and without definite inclusions. Additional findings included mild to moderate lobular inflammation and moderate macrovesicular steatosis with rare ballooned cells but no Mallory-Denk bodies. Iron stains showed reticuloendothelial deposits within Kupffer cells. AFB and GMS stains were negative. Bile ducts were intact with no florid duct lesions. These findings suggested granulomatosis secondary to injection drug use. The patient was treated symptomatically and seen by addiction psychiatry. Her liver tests remained unchanged, and her symptoms resolved with avoidance of injectable drugs. She was counseled about safe injection practices and discharged on a methadone taper with interest in inpatient rehabilitation.
Discussion: Injection drug use is a well-known risk factor for foreign body granulomatous reactions. Although it most commonly affects the skin and lungs, we must consider granulomatous reactions to foreign bodies in patients with finding suggestive of infiltrative disease in other organs such as the liver.

Disclosures:
Daniel J. Alvarez, MD, Alexander Abadir, MD, Geetika Goyal, MD, Kristina Chacko, MD. P1081 - Lodged in the Liver: A Case of Foreign Body Granulomatosis From Injection Drug Use, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Montefiore Medical Center/Albert Einstein College of Medicine, Bronx, NY
Introduction: Granulomatosis as a foreign body reaction has been described in the setting of prosthesis placement, cosmetic procedures, retained surgical debris, and injection drug use. Most commonly, granulomas involve the skin and soft tissues but may also affect the lung, liver, arachnoid membrane or occur as a systemic granulomatous reaction with multi-organ involvement. Additives such as talc have been implicated as the cause.
Case Description/Methods: The patient is a 46 year-old female who initially presented with worsening nausea, vomiting, epigastric pain, anorexia and weight loss for 2 months. Her medical history was notable for active injection drug use with opioids. Initial labs were remarkable for pancytopenia: white blood cells 2.3k/uL, hemoglobin 9.5g/dL, and platelets 47k/uL. Liver tests were notable for a cholestatic pattern with alkaline phosphatase of 2061U/L, AST of 144U/L, ALT of 70U/L, total bilirubin of 1.4, and albumin of 2.9g/dL. A gamma-glutamyl transferase was 845U/L. An extensive laboratory evaluation for autoimmune and infectious etiologies was negative. Copper levels and ceruloplasmin were normal. Abdominal imaging including CT and MRI showed hepatosplenomegaly and lymphadenopathy. Chest x-ray revealed no hilar lymphadenopathy and she had no respiratory symptoms. Transfemoral hepatic biopsy was performed. Pathology showed portal tracts with moderate lymphocytic inflammation and non-necrotizing giant cell granulomas surrounded by a lymphoid cuff and without definite inclusions. Additional findings included mild to moderate lobular inflammation and moderate macrovesicular steatosis with rare ballooned cells but no Mallory-Denk bodies. Iron stains showed reticuloendothelial deposits within Kupffer cells. AFB and GMS stains were negative. Bile ducts were intact with no florid duct lesions. These findings suggested granulomatosis secondary to injection drug use. The patient was treated symptomatically and seen by addiction psychiatry. Her liver tests remained unchanged, and her symptoms resolved with avoidance of injectable drugs. She was counseled about safe injection practices and discharged on a methadone taper with interest in inpatient rehabilitation.
Discussion: Injection drug use is a well-known risk factor for foreign body granulomatous reactions. Although it most commonly affects the skin and lungs, we must consider granulomatous reactions to foreign bodies in patients with finding suggestive of infiltrative disease in other organs such as the liver.

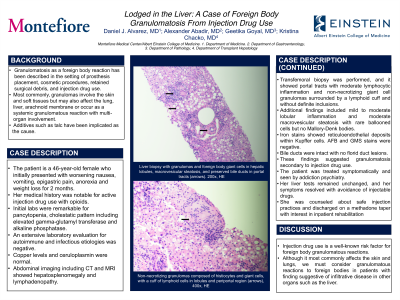
Figure: A. Liver biopsy with granulomas and foreign body giant cells in hepatic lobules, macrovesicular steatosis, and preserved bile ducts in portal tracts (arrows). 200x, HE
B. Macrovesicular steatosis in pan lobular distribution (60%), and non-necrotizing granulomas in lobules (arrows), 200x, HE
C. Non-necrotizing granulomas composed of histiocytes and giant cells, with a cuff of lymphoid cells in lobules and periportal region (arrows), 400x, HE
B. Macrovesicular steatosis in pan lobular distribution (60%), and non-necrotizing granulomas in lobules (arrows), 200x, HE
C. Non-necrotizing granulomas composed of histiocytes and giant cells, with a cuff of lymphoid cells in lobules and periportal region (arrows), 400x, HE
Disclosures:
Daniel Alvarez indicated no relevant financial relationships.
Alexander Abadir indicated no relevant financial relationships.
Geetika Goyal indicated no relevant financial relationships.
Kristina Chacko indicated no relevant financial relationships.
Daniel J. Alvarez, MD, Alexander Abadir, MD, Geetika Goyal, MD, Kristina Chacko, MD. P1081 - Lodged in the Liver: A Case of Foreign Body Granulomatosis From Injection Drug Use, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
