Sunday Poster Session
Category: Liver
P1082 - A Case of Fatal Merkel Cell Carcinoma With Metastasis to the Liver Refractory to Radiation Therapy
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Pankhuri Jha, MD
University Hospitals Cleveland Medical Center
Cleveland, OH
Presenting Author(s)
Pankhuri Jha, MD1, Adrian S. Lindsey, MD2, Anthony Post, MD2
1University Hospitals Cleveland Medical Center, Cleveland, OH; 2CWRU/UH/VA, Cleveland, OH
Introduction: Merkel cell carcinoma (MCC) is a rare, highly aggressive neuroendocrine skin tumor that presents with liver metastasis in less than eight percent of cases. We present a case of a patient who despite receiving the standard treatment for loco-regional MCC, developed systemic disease three months later with liver metastasis.
Case Description/Methods: A 64-year-old Caucasian male with a history of kidney and pancreas transplant on azathioprine and cyclosporine, basal cell carcinoma (BCC), and squamous cell carcinoma (SCC) of the skin, presented with hypovolemic shock after completing five weeks of radiation for T1N3M0 MCC. Admission labs noted an elevated Alkaline phosphatase, AST, and bilirubin. A CTAP without contrast showed a nodular liver and a heterogenous attenuation of the liver parenchyma without splenomegaly or ascites. Cirrhosis work-up was unrevealing. MRI liver with contrast showed near complete parenchymal replacement with T1 hypointense and T2 hyperintense lesions, the largest measuring 2 cm x 1.8 cm. Liver biopsy confirmed metastatic MCC. The hospital course was complicated by worsening renal function requiring dialysis. Due to poor prognosis, the patient chose comfort care and expired four days later.
The patient was first diagnosed with MCC in September 2022, after presenting with a lesion on his right lower abdomen. He underwent a wide local excision with sentinel node biopsy which revealed negative margins and a positive right iliac inguinal node with both MCC and SCC. A post-operative PET/CT on 10/21/22 was negative for distant metastasis. Five weeks of daily radiation was completed on 12/20/22.
Discussion: At diagnosis of MCC, loco-regional metastasis is present in 30% of patients. For such lesions, treatment is wide local excision and adjunctive radiation. However, the utility of radiation is speculative, as some studies suggest no association between radiation and recurrence, especially in those with margin-negative excisions. Other studies show reduced rates of recurrence and improved survival after radiation. Further, few cases of MCC develop infiltrative liver disease. The mean latency period from MCC diagnosis to systemic metastasis is 2.1 years. In this case, liver metastasis occurred within three months. To date, only one other case has reported radiation refractory loco-regional MCC with liver metastasis resulting in death. This case highlights that although it is rare for MCC to spread to the liver, it can happen rapidly, and can occur despite radiation therapy.

Disclosures:
Pankhuri Jha, MD1, Adrian S. Lindsey, MD2, Anthony Post, MD2. P1082 - A Case of Fatal Merkel Cell Carcinoma With Metastasis to the Liver Refractory to Radiation Therapy, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University Hospitals Cleveland Medical Center, Cleveland, OH; 2CWRU/UH/VA, Cleveland, OH
Introduction: Merkel cell carcinoma (MCC) is a rare, highly aggressive neuroendocrine skin tumor that presents with liver metastasis in less than eight percent of cases. We present a case of a patient who despite receiving the standard treatment for loco-regional MCC, developed systemic disease three months later with liver metastasis.
Case Description/Methods: A 64-year-old Caucasian male with a history of kidney and pancreas transplant on azathioprine and cyclosporine, basal cell carcinoma (BCC), and squamous cell carcinoma (SCC) of the skin, presented with hypovolemic shock after completing five weeks of radiation for T1N3M0 MCC. Admission labs noted an elevated Alkaline phosphatase, AST, and bilirubin. A CTAP without contrast showed a nodular liver and a heterogenous attenuation of the liver parenchyma without splenomegaly or ascites. Cirrhosis work-up was unrevealing. MRI liver with contrast showed near complete parenchymal replacement with T1 hypointense and T2 hyperintense lesions, the largest measuring 2 cm x 1.8 cm. Liver biopsy confirmed metastatic MCC. The hospital course was complicated by worsening renal function requiring dialysis. Due to poor prognosis, the patient chose comfort care and expired four days later.
The patient was first diagnosed with MCC in September 2022, after presenting with a lesion on his right lower abdomen. He underwent a wide local excision with sentinel node biopsy which revealed negative margins and a positive right iliac inguinal node with both MCC and SCC. A post-operative PET/CT on 10/21/22 was negative for distant metastasis. Five weeks of daily radiation was completed on 12/20/22.
Discussion: At diagnosis of MCC, loco-regional metastasis is present in 30% of patients. For such lesions, treatment is wide local excision and adjunctive radiation. However, the utility of radiation is speculative, as some studies suggest no association between radiation and recurrence, especially in those with margin-negative excisions. Other studies show reduced rates of recurrence and improved survival after radiation. Further, few cases of MCC develop infiltrative liver disease. The mean latency period from MCC diagnosis to systemic metastasis is 2.1 years. In this case, liver metastasis occurred within three months. To date, only one other case has reported radiation refractory loco-regional MCC with liver metastasis resulting in death. This case highlights that although it is rare for MCC to spread to the liver, it can happen rapidly, and can occur despite radiation therapy.

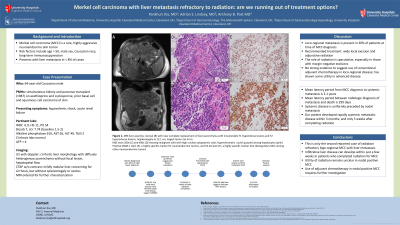
Figure: MRI liver axial (A), coronal (B) with near complete replacement of liver parenchyma with innumerable T1 hypointense lesions and T2 hyperintense lesions.
H&E stain 200x (C) and 400x (D) showing malignant Merkel cells with a high nuclear:cytoplasmic ratio and hyperchromatic nuclei (purple) among hepatocytes (pink).
Positive INSM-1 stain (E), a highly specific marker for neuroendocrine tumors, and CK-20 stain (F), a highly specific marker that distinguishes Merkel cell carcinoma among other neuroendocrine tumors.
H&E stain 200x (C) and 400x (D) showing malignant Merkel cells with a high nuclear:cytoplasmic ratio and hyperchromatic nuclei (purple) among hepatocytes (pink).
Positive INSM-1 stain (E), a highly specific marker for neuroendocrine tumors, and CK-20 stain (F), a highly specific marker that distinguishes Merkel cell carcinoma among other neuroendocrine tumors.
Disclosures:
Pankhuri Jha indicated no relevant financial relationships.
Adrian Lindsey indicated no relevant financial relationships.
Anthony Post indicated no relevant financial relationships.
Pankhuri Jha, MD1, Adrian S. Lindsey, MD2, Anthony Post, MD2. P1082 - A Case of Fatal Merkel Cell Carcinoma With Metastasis to the Liver Refractory to Radiation Therapy, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

