Sunday Poster Session
Category: Liver
P1089 - Not a Fad Diet: Using Weight Loss Through Bariatric Surgery to Prevent Liver Transplantation in Hepatic Adenoma
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio
Kyle Scholten, DO
University of Nebraska Medical Center
Omaha, NE
Presenting Author(s)
Kyle Scholten, DO, Kevin Brittan, MD, Patrick Twohig, MD, MPH, Jason Barbaretta, MD, Wendy Grant, MD, Thoetchai Peeraphatdit, MD
University of Nebraska Medical Center, Omaha, NE
Introduction: Hepatocellular adenoma (HCA) is a benign solid tumor of the liver traditionally linked to oral contraceptive pills, obesity, and metabolic syndrome. Although considered benign, there is a risk of hemorrhage and malignant transformation. Treatment for asymptomatic lesions less than 5 cm includes discontinuing exogenous hormones and weight loss. In symptomatic patients or lesions > 5cm, transarterial embolization (TAE), surgical resection, and/or liver transplantation are definitive treatments. Recent studies suggest that weight loss surgery may significantly reduce the size of HCA, foregoing the need for liver transplant. We describe a case of symptomatic HCA treated successfully with the combination of sleeve gastrectomy and TAE to achieve remission and prevent liver transplantation.
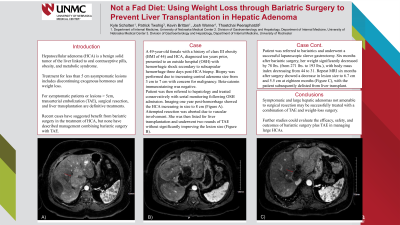
Case Description/Methods: A 49-year-old female with a history of morbid obesity with BMI of 44 and HCA presented to an outside hospital (OSH) with hemorrhagic shock secondary to subcapsular hemorrhage three days post-HCA biopsy. Biopsy was performed due to increasing central adenoma size from 3 cm to 7 cm. Beta-catenin immunostaining was negative. Patient was treated conservatively and underwent serial monitoring following OSH admission. She then presented in 2021 with abdominal pain. CT scan showed recurrent HCA measuring 8.3 x 6.3 cm. Attempted resection was aborted due to vascular involvement. She was listed for liver transplantation and underwent two rounds of TAE without significantly improving the lesion size. Following this, she underwent sleeve gastrectomy with a reduction in BMI from 44 to 31. Repeat MRI in April 2022 showed a decrease in lesion size from 8.3 x 6.1 to 6.7 x 4.2 cm (Figure 1). Consequently, patient was delisted for liver transplant.
Discussion: Symptomatic and/or large hepatic adenomas not amenable to surgical resection may be successfully treated with a combination of TAE and weight-loss surgery. Although TAE has primarily been a modality to treat bleeding HCAs, it is now utilized to promote tumor regression for non-bleeding HCAs. Likewise, weight loss through bariatric surgery may be a good treatment option regardless of any other treatment modality used for HCAs (e.g., surgical resection, TAE, or transplant), given the impact that weight loss has on overall health and minimizing the development of a myriad of health conditions related to a lifetime of morbid obesity. Further studies could evaluate the efficacy, safety, and outcomes of bariatric surgery + TAE in managing large HCAs.

Disclosures:
Kyle Scholten, DO, Kevin Brittan, MD, Patrick Twohig, MD, MPH, Jason Barbaretta, MD, Wendy Grant, MD, Thoetchai Peeraphatdit, MD. P1089 - Not a Fad Diet: Using Weight Loss Through Bariatric Surgery to Prevent Liver Transplantation in Hepatic Adenoma, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
University of Nebraska Medical Center, Omaha, NE
Introduction: Hepatocellular adenoma (HCA) is a benign solid tumor of the liver traditionally linked to oral contraceptive pills, obesity, and metabolic syndrome. Although considered benign, there is a risk of hemorrhage and malignant transformation. Treatment for asymptomatic lesions less than 5 cm includes discontinuing exogenous hormones and weight loss. In symptomatic patients or lesions > 5cm, transarterial embolization (TAE), surgical resection, and/or liver transplantation are definitive treatments. Recent studies suggest that weight loss surgery may significantly reduce the size of HCA, foregoing the need for liver transplant. We describe a case of symptomatic HCA treated successfully with the combination of sleeve gastrectomy and TAE to achieve remission and prevent liver transplantation.
Case Description/Methods: A 49-year-old female with a history of morbid obesity with BMI of 44 and HCA presented to an outside hospital (OSH) with hemorrhagic shock secondary to subcapsular hemorrhage three days post-HCA biopsy. Biopsy was performed due to increasing central adenoma size from 3 cm to 7 cm. Beta-catenin immunostaining was negative. Patient was treated conservatively and underwent serial monitoring following OSH admission. She then presented in 2021 with abdominal pain. CT scan showed recurrent HCA measuring 8.3 x 6.3 cm. Attempted resection was aborted due to vascular involvement. She was listed for liver transplantation and underwent two rounds of TAE without significantly improving the lesion size. Following this, she underwent sleeve gastrectomy with a reduction in BMI from 44 to 31. Repeat MRI in April 2022 showed a decrease in lesion size from 8.3 x 6.1 to 6.7 x 4.2 cm (Figure 1). Consequently, patient was delisted for liver transplant.
Discussion: Symptomatic and/or large hepatic adenomas not amenable to surgical resection may be successfully treated with a combination of TAE and weight-loss surgery. Although TAE has primarily been a modality to treat bleeding HCAs, it is now utilized to promote tumor regression for non-bleeding HCAs. Likewise, weight loss through bariatric surgery may be a good treatment option regardless of any other treatment modality used for HCAs (e.g., surgical resection, TAE, or transplant), given the impact that weight loss has on overall health and minimizing the development of a myriad of health conditions related to a lifetime of morbid obesity. Further studies could evaluate the efficacy, safety, and outcomes of bariatric surgery + TAE in managing large HCAs.

Figure: Split figure, with T2 Flair MRI Imaging, A) showing the HCA pre-weight loss surgery and B) after weight loss surgery
Disclosures:
Kyle Scholten indicated no relevant financial relationships.
Kevin Brittan indicated no relevant financial relationships.
Patrick Twohig: Bausch Health – Grant/Research Support.
Jason Barbaretta indicated no relevant financial relationships.
Wendy Grant indicated no relevant financial relationships.
Thoetchai Peeraphatdit indicated no relevant financial relationships.
Kyle Scholten, DO, Kevin Brittan, MD, Patrick Twohig, MD, MPH, Jason Barbaretta, MD, Wendy Grant, MD, Thoetchai Peeraphatdit, MD. P1089 - Not a Fad Diet: Using Weight Loss Through Bariatric Surgery to Prevent Liver Transplantation in Hepatic Adenoma, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
