Sunday Poster Session
Category: Liver
P1090 - Fortune Favors the Bold: Successful Treatment of Post-Liver Transplant Lymphoproliferative Disorder Using High-Dose Methotrexate
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio
Kyle Scholten, DO
University of Nebraska Medical Center
Omaha, NE
Presenting Author(s)
Kyle Scholten, DO1, Kevin Brittan, MD1, Jason Barbaretta, MD1, Patrick Twohig, MD, MPH1, Faruq Pradhan, MBBCh1, Neha Gupta, MBBS1, Tomoki Sempokuya, MD2, Wuttiporn Manatsathit, MD1
1University of Nebraska Medical Center, Omaha, NE; 2University of Nebraska Medical Center, Honolulu, HI
Introduction: Post-transplant lymphoproliferative disorder (PTLD) is a malignancy that occurs in 2-20% of solid organ transplant recipients. Isolated, primary central nervous system (PCNS) PTLD is exceedingly rare, with existing data limited to case reports and case series. PCNS PTLD is difficult to diagnose given 1) non-specific clinical presentation and 2) burden of immunosuppression broadens differential diagnoses, often requiring extensive testing and delays in treatment. PTLD is typically treated with systemic chemotherapy, however, this does not cross the blood-brain barrier. As a result, PCNS PTLD is treated with methotrexate, a notoriously hepatotoxic agent. Although reports of successful treatment with methotrexate exist in kidney transplant recipients, its use in liver transplant recipients is sparsely reported. We present a rare case of post-liver transplant PCNS PTLD successfully treated with high-dose methotrexate.
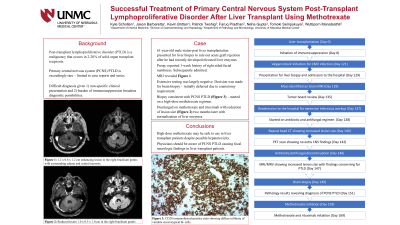
Case Description/Methods: A 61-year-old male 4-month status-post liver transplantation presented for liver biopsy due to elevated liver enzymes. Preoperatively, he reported acute right-sided facial numbness and weakness and was subsequently admitted for further workup. Magnetic resonance imaging (MRI) of the brain with contrast revealed a 1.2 x 0.8 x 1.2 cm enhancing lesion in the right brachium pontis with surrounding edema and central necrosis (Figure 1). A brain biopsy revealed PCNS PTLD. High-dose methotrexate regimen was started, and he was ultimately discharged on methotrexate and rituximab. Two months after starting treatment, an MRI showed a reduction in lesion size. His liver function remains normal, with no evidence of hepatotoxicity secondary to methotrexate therapy.
Discussion: Though uncommon, physicians should be aware of PCNS PTLD as a potential cause of focal neurologic deficits after solid organ transplantation. Our case demonstrates that high-dose methotrexate may be a safe treatment option in liver transplant recipients despite its association with hepatotoxicity.

Disclosures:
Kyle Scholten, DO1, Kevin Brittan, MD1, Jason Barbaretta, MD1, Patrick Twohig, MD, MPH1, Faruq Pradhan, MBBCh1, Neha Gupta, MBBS1, Tomoki Sempokuya, MD2, Wuttiporn Manatsathit, MD1. P1090 - Fortune Favors the Bold: Successful Treatment of Post-Liver Transplant Lymphoproliferative Disorder Using High-Dose Methotrexate, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Nebraska Medical Center, Omaha, NE; 2University of Nebraska Medical Center, Honolulu, HI
Introduction: Post-transplant lymphoproliferative disorder (PTLD) is a malignancy that occurs in 2-20% of solid organ transplant recipients. Isolated, primary central nervous system (PCNS) PTLD is exceedingly rare, with existing data limited to case reports and case series. PCNS PTLD is difficult to diagnose given 1) non-specific clinical presentation and 2) burden of immunosuppression broadens differential diagnoses, often requiring extensive testing and delays in treatment. PTLD is typically treated with systemic chemotherapy, however, this does not cross the blood-brain barrier. As a result, PCNS PTLD is treated with methotrexate, a notoriously hepatotoxic agent. Although reports of successful treatment with methotrexate exist in kidney transplant recipients, its use in liver transplant recipients is sparsely reported. We present a rare case of post-liver transplant PCNS PTLD successfully treated with high-dose methotrexate.
Case Description/Methods: A 61-year-old male 4-month status-post liver transplantation presented for liver biopsy due to elevated liver enzymes. Preoperatively, he reported acute right-sided facial numbness and weakness and was subsequently admitted for further workup. Magnetic resonance imaging (MRI) of the brain with contrast revealed a 1.2 x 0.8 x 1.2 cm enhancing lesion in the right brachium pontis with surrounding edema and central necrosis (Figure 1). A brain biopsy revealed PCNS PTLD. High-dose methotrexate regimen was started, and he was ultimately discharged on methotrexate and rituximab. Two months after starting treatment, an MRI showed a reduction in lesion size. His liver function remains normal, with no evidence of hepatotoxicity secondary to methotrexate therapy.
Discussion: Though uncommon, physicians should be aware of PCNS PTLD as a potential cause of focal neurologic deficits after solid organ transplantation. Our case demonstrates that high-dose methotrexate may be a safe treatment option in liver transplant recipients despite its association with hepatotoxicity.

Figure: Initial MRI with Axial T1 3D (left) and Axial T2 Flair (right).
Disclosures:
Kyle Scholten indicated no relevant financial relationships.
Kevin Brittan indicated no relevant financial relationships.
Jason Barbaretta indicated no relevant financial relationships.
Patrick Twohig: Bausch Health – Grant/Research Support.
Faruq Pradhan indicated no relevant financial relationships.
Neha Gupta indicated no relevant financial relationships.
Tomoki Sempokuya indicated no relevant financial relationships.
Wuttiporn Manatsathit indicated no relevant financial relationships.
Kyle Scholten, DO1, Kevin Brittan, MD1, Jason Barbaretta, MD1, Patrick Twohig, MD, MPH1, Faruq Pradhan, MBBCh1, Neha Gupta, MBBS1, Tomoki Sempokuya, MD2, Wuttiporn Manatsathit, MD1. P1090 - Fortune Favors the Bold: Successful Treatment of Post-Liver Transplant Lymphoproliferative Disorder Using High-Dose Methotrexate, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
