Sunday Poster Session
Category: Liver
P1098 - Shrouded Secrets: The Mysterious Saga of Yersinia enterocolitica Bacteremia and the Veiled Hepatic Abscess
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Udit Asija, MD
The Wright Center for GME
DUNMORE, PA
Presenting Author(s)
Udit Asija, MD1, Chilsia Shafi, MBBS2, Mashu Shrivastava, MBBS2, Khalid Ahmed, MD1, Peter Iskander, MD3, Gary Decker, MD2
1The Wright Center for GME, Scranton, PA; 2The Wright Center for Graduate Medical Education, Scranton, PA; 3The Wright Center for GME, Dunmore, PA
Introduction: Yersinia enterocolitica is a foodborne gram-negative bacillus that infects after ingestion of contaminated food (uncooked meat products) or water or by direct inoculation through blood transfusion usually causing enterocolitis, mesenteric lymphadenitis, and terminal ileitis thereby mimicking appendicitis or Crohn's disease[2]. Yersinia bacteremia with hepatic abscesses is rarely seen and even rarer to encounter in an immunocompetent host(4).
Case Description/Methods: 55-year-old male with past history of hypertension presented with right-sided abdominal pain, yellowish discoloration of skin and eyes, and 40 lbs weight loss over past 4 weeks. Lab work revealed leukocytosis, ALP 205 unit/L, ALT 71 unit/L, AST 67 unit/L, Total bilirubin 5.22 mg/dL, elevated CRP 98.00 mg/L. CECT and MRI with contrast abdomen revealed 15.5 x 13.8 x 16.1 cm multilobulated mass in the porta hepatis extending to the upper, lower right lobe, and left lobe, causing mass effect on hepatic vasculature. Tumor markers (AFP, CA 19-9, and CEA) were within normal limits and hepatitis panel was negative. Attempt at Interventional radiology guided biopsy revealed pustular discharge and thus underwent CT-guided abscess drainage of 550 mL pus with percutaneous catheter placement. Blood cultures as well as liver abscess aspirate grew Y.enterocolitica. Colonoscopy revealed biopsy confirmed deep ulcerations in the terminal ileum, ascending, and transverse colon. Patient was started on high-dose IV Ceftriaxone and oral metronidazole later transitioned to oral levofloxacin and metronidazole for 4-6 weeks which led to clinical improvement and negative repeat blood cultures. The patient was planned for serial CT scans on outpatient basis and repeat colonoscopy to assess for resolution of intestinal ulcers.
Discussion: Y. Enterocolitica septicemia is extremely rare to be encountered in immunocompetent patients (as in our case) and is mostly seen in patient with immunosuppression or with iron overload pathologies (hemochromatosis, thalassemias, etc) as most subtypes of the organism lack genes for iron uptake(1)(3)(4). Given the fact that most bacteremic hepatic abscesses originate through the hematogenous seeding from portal circulation implies some sort of mucosal disruption of the intestinal tract and thus every patient with bacteremic hepatic abscess should undergo upper and lower endoscopy for further evaluation. Treatment involves source control with percutaneous drainage, long-term antibiotics, and serial imaging to ensure resolution.

Disclosures:
Udit Asija, MD1, Chilsia Shafi, MBBS2, Mashu Shrivastava, MBBS2, Khalid Ahmed, MD1, Peter Iskander, MD3, Gary Decker, MD2. P1098 - Shrouded Secrets: The Mysterious Saga of Yersinia enterocolitica Bacteremia and the Veiled Hepatic Abscess, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1The Wright Center for GME, Scranton, PA; 2The Wright Center for Graduate Medical Education, Scranton, PA; 3The Wright Center for GME, Dunmore, PA
Introduction: Yersinia enterocolitica is a foodborne gram-negative bacillus that infects after ingestion of contaminated food (uncooked meat products) or water or by direct inoculation through blood transfusion usually causing enterocolitis, mesenteric lymphadenitis, and terminal ileitis thereby mimicking appendicitis or Crohn's disease[2]. Yersinia bacteremia with hepatic abscesses is rarely seen and even rarer to encounter in an immunocompetent host(4).
Case Description/Methods: 55-year-old male with past history of hypertension presented with right-sided abdominal pain, yellowish discoloration of skin and eyes, and 40 lbs weight loss over past 4 weeks. Lab work revealed leukocytosis, ALP 205 unit/L, ALT 71 unit/L, AST 67 unit/L, Total bilirubin 5.22 mg/dL, elevated CRP 98.00 mg/L. CECT and MRI with contrast abdomen revealed 15.5 x 13.8 x 16.1 cm multilobulated mass in the porta hepatis extending to the upper, lower right lobe, and left lobe, causing mass effect on hepatic vasculature. Tumor markers (AFP, CA 19-9, and CEA) were within normal limits and hepatitis panel was negative. Attempt at Interventional radiology guided biopsy revealed pustular discharge and thus underwent CT-guided abscess drainage of 550 mL pus with percutaneous catheter placement. Blood cultures as well as liver abscess aspirate grew Y.enterocolitica. Colonoscopy revealed biopsy confirmed deep ulcerations in the terminal ileum, ascending, and transverse colon. Patient was started on high-dose IV Ceftriaxone and oral metronidazole later transitioned to oral levofloxacin and metronidazole for 4-6 weeks which led to clinical improvement and negative repeat blood cultures. The patient was planned for serial CT scans on outpatient basis and repeat colonoscopy to assess for resolution of intestinal ulcers.
Discussion: Y. Enterocolitica septicemia is extremely rare to be encountered in immunocompetent patients (as in our case) and is mostly seen in patient with immunosuppression or with iron overload pathologies (hemochromatosis, thalassemias, etc) as most subtypes of the organism lack genes for iron uptake(1)(3)(4). Given the fact that most bacteremic hepatic abscesses originate through the hematogenous seeding from portal circulation implies some sort of mucosal disruption of the intestinal tract and thus every patient with bacteremic hepatic abscess should undergo upper and lower endoscopy for further evaluation. Treatment involves source control with percutaneous drainage, long-term antibiotics, and serial imaging to ensure resolution.

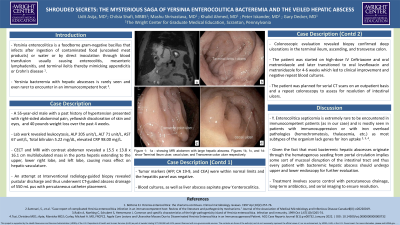
Figure: Figure a - showing MRI abdomen with large hepatic abscess. Figure b, c, and d-
showing Terminal Ileum ulcer, cecal ulcer, and Transverse colon ulcer respectively.
showing Terminal Ileum ulcer, cecal ulcer, and Transverse colon ulcer respectively.
Disclosures:
Udit Asija indicated no relevant financial relationships.
Chilsia Shafi indicated no relevant financial relationships.
Mashu Shrivastava indicated no relevant financial relationships.
Khalid Ahmed indicated no relevant financial relationships.
Peter Iskander indicated no relevant financial relationships.
Gary Decker indicated no relevant financial relationships.
Udit Asija, MD1, Chilsia Shafi, MBBS2, Mashu Shrivastava, MBBS2, Khalid Ahmed, MD1, Peter Iskander, MD3, Gary Decker, MD2. P1098 - Shrouded Secrets: The Mysterious Saga of Yersinia enterocolitica Bacteremia and the Veiled Hepatic Abscess, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
