Sunday Poster Session
Category: Liver
P1108 - Apixaban Failure in Idiopathic Budd-Chiari Syndrome
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Cheng-Hung Tai, MD
Yale New Haven Health/Bridgeport Hospital
Bridgeport, CT
Presenting Author(s)
Cheng-Hung Tai, MD1, Prince Addo. Ameyaw, MD2, Jamil O. Alexis, MD2, Michael H. Nathanson, MD, PhD3
1Yale New Haven Health/Bridgeport Hospital, Bridgeport, CT; 2Bridgeport Hospital/Yale New Haven Health, Bridgeport, CT; 3Yale School of Medicine, New Haven, CT
Introduction: Primary Budd-Chiari syndrome (BCS) is a rare disease characterized by hepatic venous obstruction resulting from thrombosis and often associated with other syndromes with hypercoagulability. Approximately 20% of cases are deemed idiopathic after extensive evaluation for prothrombotic disease. Here we present a challenging case of BCS refractory to apixaban.
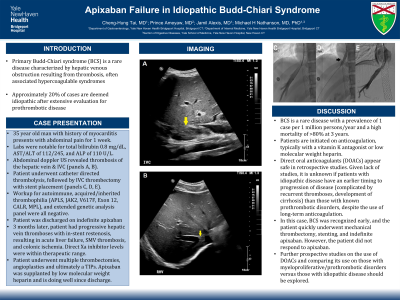
Case Description/Methods: A 35 year old with history of myocarditis presents with a 1 week history of abdominal pain. Vitals were stable. Labs were notable for total bilirubin 0.8 mg/dL, AST/ALT of 112/245, and ALP of 110 U/L. Abdominal doppler ultrasound revealed occlusive thrombosis of the hepatic vein and IVC (panels A, B). Patient was started on heparin and underwent catheter directed thrombolysis, followed by IVC thrombectomy with stent placement (panels C, D, E). Workup for autoimmune, acquired/inherited thrombophilia (APLS, JAK2, V617F, Exon 12, CALR, MPL), and an extended genetic analysis panel were all negative. Patient was discharged on indefinite apixaban. 3 months later, patient was readmitted for progressive hepatic vein thromboses with in-stent restenosis resulting in acute liver failure, SMV thrombosis, and colonic ischemia with 3 exploratory laparotomies. Direct Xa inhibitor levels were within therapeutic range. Patient underwent multiple rounds of thrombectomies, angioplasties and ultimately a TIPs. Apixaban was supplanted by low molecular weight heparin and is doing well since discharge.
Discussion: BCS is a rare disease with a prevalence of 1 case per 1 million persons/year and a high mortality of >80% at 3 years. Early disease recognition with restoration of hepatic venous outflow is crucial. Patients are initiated on anticoagulation, typically with a vitamin K antagonist or low molecular weight heparin. Direct oral anticoagulants (DOACs) appear safe in retrospective studies. Given lack of studies, it is unknown if patients with idiopathic disease have an earlier timing to progression of disease (complicated by recurrent thromboses, development of cirrhosis) than those with known prothrombotic disorders, despite the use of long-term anticoagulation. In this case, BCS was recognized early, and the patient quickly underwent mechanical thrombectomy, stenting, and indefinite apixaban. However, the patient did not respond to apixaban. Further prospective studies on the use of DOACs and comparing its use on those with myeloproliferative/prothrombotic disorders versus those with idiopathic disease should be explored.

Disclosures:
Cheng-Hung Tai, MD1, Prince Addo. Ameyaw, MD2, Jamil O. Alexis, MD2, Michael H. Nathanson, MD, PhD3. P1108 - Apixaban Failure in Idiopathic Budd-Chiari Syndrome, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Yale New Haven Health/Bridgeport Hospital, Bridgeport, CT; 2Bridgeport Hospital/Yale New Haven Health, Bridgeport, CT; 3Yale School of Medicine, New Haven, CT
Introduction: Primary Budd-Chiari syndrome (BCS) is a rare disease characterized by hepatic venous obstruction resulting from thrombosis and often associated with other syndromes with hypercoagulability. Approximately 20% of cases are deemed idiopathic after extensive evaluation for prothrombotic disease. Here we present a challenging case of BCS refractory to apixaban.
Case Description/Methods: A 35 year old with history of myocarditis presents with a 1 week history of abdominal pain. Vitals were stable. Labs were notable for total bilirubin 0.8 mg/dL, AST/ALT of 112/245, and ALP of 110 U/L. Abdominal doppler ultrasound revealed occlusive thrombosis of the hepatic vein and IVC (panels A, B). Patient was started on heparin and underwent catheter directed thrombolysis, followed by IVC thrombectomy with stent placement (panels C, D, E). Workup for autoimmune, acquired/inherited thrombophilia (APLS, JAK2, V617F, Exon 12, CALR, MPL), and an extended genetic analysis panel were all negative. Patient was discharged on indefinite apixaban. 3 months later, patient was readmitted for progressive hepatic vein thromboses with in-stent restenosis resulting in acute liver failure, SMV thrombosis, and colonic ischemia with 3 exploratory laparotomies. Direct Xa inhibitor levels were within therapeutic range. Patient underwent multiple rounds of thrombectomies, angioplasties and ultimately a TIPs. Apixaban was supplanted by low molecular weight heparin and is doing well since discharge.
Discussion: BCS is a rare disease with a prevalence of 1 case per 1 million persons/year and a high mortality of >80% at 3 years. Early disease recognition with restoration of hepatic venous outflow is crucial. Patients are initiated on anticoagulation, typically with a vitamin K antagonist or low molecular weight heparin. Direct oral anticoagulants (DOACs) appear safe in retrospective studies. Given lack of studies, it is unknown if patients with idiopathic disease have an earlier timing to progression of disease (complicated by recurrent thromboses, development of cirrhosis) than those with known prothrombotic disorders, despite the use of long-term anticoagulation. In this case, BCS was recognized early, and the patient quickly underwent mechanical thrombectomy, stenting, and indefinite apixaban. However, the patient did not respond to apixaban. Further prospective studies on the use of DOACs and comparing its use on those with myeloproliferative/prothrombotic disorders versus those with idiopathic disease should be explored.

Figure: A, B: Abdominal doppler ultrasound depicting thrombus in IVC, hepatic vein; C, D, E: IR venogram with stent and angioplasty
Disclosures:
Cheng-Hung Tai indicated no relevant financial relationships.
Prince Ameyaw indicated no relevant financial relationships.
Jamil Alexis indicated no relevant financial relationships.
Michael Nathanson indicated no relevant financial relationships.
Cheng-Hung Tai, MD1, Prince Addo. Ameyaw, MD2, Jamil O. Alexis, MD2, Michael H. Nathanson, MD, PhD3. P1108 - Apixaban Failure in Idiopathic Budd-Chiari Syndrome, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

