Sunday Poster Session
Category: Liver
P1116 - Difference Between Life and Death: Oral Amiodarone-Induced Reversible Acute Liver Failure
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Patrick Tempera, DO
Albany Medical Center
Albany, NY
Presenting Author(s)
Patrick Tempera, DO1, Ahmad Abulawi, MBBS2, Raya Alashram, MD1, Amit Chopra, MD1
1Albany Medical Center, Albany, NY; 2Albany Medical College, Albany, NY
Introduction: Amiodarone is a highly effective treatment for supraventricular and ventricular tachyarrhythmias. However, in rare instances, it can be associated with serious adverse events, such as acute liver failure. We describe the case of a 71-year-old male with oral amiodarone induced hepatotoxicity resulting in cirrhosis and decompensated hepatic failure.
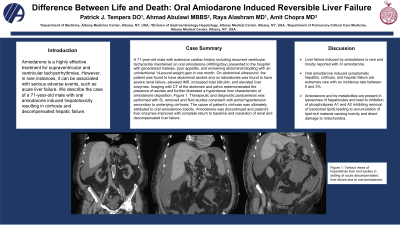
Case Description/Methods: A 71-year-old male with extensive cardiac history including recurrent ventricular tachycardia maintained on oral amiodarone (400mg/day) presented to the hospital with generalized malaise, poor appetite, and worsening abdominal bloating with an unintentional 14-pound weight gain in one month. On abdominal ultrasound, the patient was found to have abdominal ascites and on laboratories was found to have severe renal failure, elevated INR, increased total bilirubin, and elevated liver enzymes. Imaging with CT of the abdomen and pelvis redemonstrated the presence of ascites and further illustrated a hyperdense liver characteristic of amiodarone deposition, Figure 1. Therapeutic and diagnostic paracentesis was performed with 5L removed and fluid studies consistent with portal hypertension secondary to underlying cirrhosis. The cause of patient’s cirrhosis was ultimately attributed to oral amiodarone toxicity. Amiodarone was discontinued and patient’s liver enzymes improved with complete return to baseline and resolution of renal and decompensated liver failure.
Discussion: In this report, we present the clinical features of a patient with oral amiodarone induced hepatotoxicity that progressed to cirrhosis and decompensated liver failure with reversal of acute liver failure after cessation of the insulting medication. Liver failure induced by amiodarone is rare and mostly reported with IV amiodarone. Oral amiodarone induced symptomatic hepatitis, cirrhosis, and hepatic failure are extremely rare with an incidence rate between 0 and 3%. Amiodarone and its metabolites are present in lysosomes of hepatocytes and lead to inhibition of phospholipase A1 and A2 inhibiting removal of lysosomal lipids leading to accumulation of lipid-rich material causing toxicity and direct damage to mitochondria. It is important to recognize that individuals on long-term oral amiodarone are at increased risk for hepatotoxicity and identification and discontinuation of amiodarone immediately can mean the difference between life and death.

Disclosures:
Patrick Tempera, DO1, Ahmad Abulawi, MBBS2, Raya Alashram, MD1, Amit Chopra, MD1. P1116 - Difference Between Life and Death: Oral Amiodarone-Induced Reversible Acute Liver Failure, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Albany Medical Center, Albany, NY; 2Albany Medical College, Albany, NY
Introduction: Amiodarone is a highly effective treatment for supraventricular and ventricular tachyarrhythmias. However, in rare instances, it can be associated with serious adverse events, such as acute liver failure. We describe the case of a 71-year-old male with oral amiodarone induced hepatotoxicity resulting in cirrhosis and decompensated hepatic failure.
Case Description/Methods: A 71-year-old male with extensive cardiac history including recurrent ventricular tachycardia maintained on oral amiodarone (400mg/day) presented to the hospital with generalized malaise, poor appetite, and worsening abdominal bloating with an unintentional 14-pound weight gain in one month. On abdominal ultrasound, the patient was found to have abdominal ascites and on laboratories was found to have severe renal failure, elevated INR, increased total bilirubin, and elevated liver enzymes. Imaging with CT of the abdomen and pelvis redemonstrated the presence of ascites and further illustrated a hyperdense liver characteristic of amiodarone deposition, Figure 1. Therapeutic and diagnostic paracentesis was performed with 5L removed and fluid studies consistent with portal hypertension secondary to underlying cirrhosis. The cause of patient’s cirrhosis was ultimately attributed to oral amiodarone toxicity. Amiodarone was discontinued and patient’s liver enzymes improved with complete return to baseline and resolution of renal and decompensated liver failure.
Discussion: In this report, we present the clinical features of a patient with oral amiodarone induced hepatotoxicity that progressed to cirrhosis and decompensated liver failure with reversal of acute liver failure after cessation of the insulting medication. Liver failure induced by amiodarone is rare and mostly reported with IV amiodarone. Oral amiodarone induced symptomatic hepatitis, cirrhosis, and hepatic failure are extremely rare with an incidence rate between 0 and 3%. Amiodarone and its metabolites are present in lysosomes of hepatocytes and lead to inhibition of phospholipase A1 and A2 inhibiting removal of lysosomal lipids leading to accumulation of lipid-rich material causing toxicity and direct damage to mitochondria. It is important to recognize that individuals on long-term oral amiodarone are at increased risk for hepatotoxicity and identification and discontinuation of amiodarone immediately can mean the difference between life and death.

Figure: Various views of hyperdense liver and ascites in setting of acute decompensated liver failure due to oral amiodarone.
Disclosures:
Patrick Tempera indicated no relevant financial relationships.
Ahmad Abulawi indicated no relevant financial relationships.
Raya Alashram indicated no relevant financial relationships.
Amit Chopra indicated no relevant financial relationships.
Patrick Tempera, DO1, Ahmad Abulawi, MBBS2, Raya Alashram, MD1, Amit Chopra, MD1. P1116 - Difference Between Life and Death: Oral Amiodarone-Induced Reversible Acute Liver Failure, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
