Sunday Poster Session
Category: Liver
P1117 - The Role of CFTR Modulators After Liver Transplantation in Patients with Cystic Fibrosis
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio
.jpg)
Richard Maradiaga, MD
Ohio State University Wexner Medical Center
Columbus, OH
Presenting Author(s)
Richard Maradiaga, MD1, Mitchell Ramsey, MD2, Lindsay A. Sobotka, DO2
1Ohio State University Wexner Medical Center, Columbus, OH; 2The Ohio State Wexner Medical Center, Columbus, OH
Introduction: Cystic Fibrosis Transmembrane Conductance Regulator (CFTR) modulators have improved pulmonary outcomes for persons with cystic fibrosis (PwCF). Gastrointestinal manifestations of CF, including cystic fibrosis-related liver disease (CFRLD), are becoming a leading cause of morbidity and mortality in patients with CF—however, the use of CFTR modulators in decompensated cirrhosis and after liver transplantation has not been determined. We present a PwCF who underwent liver transplantation and safely resumed CFTR modulator afterward.
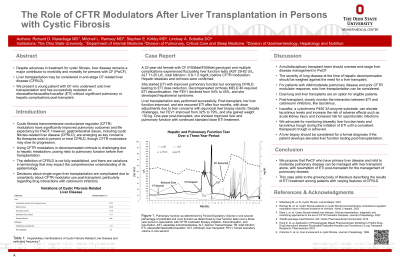
Case Description/Methods: A 22-year-old female with CF (F508del/F508del) complicated by mild CFRLD commenced elexacaftor/tezacaftor/ivacaftor (ETI) at standard dosing and experienced improved pulmonary function. However, her CFRLD progressed over time, and she developed ascites which was managed with diuretics and discontinuation of ETI. Unfortunately, her forced expiratory volume (FEV1) decreased from 54% to 45%, and she endured multiple hospitalizations due to pulmonary exacerbations. Her CFRLD continued to decompensate, developing hepatorenal syndrome requiring intermittent hemodialysis. Her MELD-Na score acutely increased to 40. Our multi-disciplinary transplant committee reviewed her case and jointly agreed to proceed with liver transplantation alone, anticipating improved pulmonary function upon future ETI reinstatement.
Her post-transplant immunosuppression included steroid induction, Cellcept, and tacrolimus with a goal trough between 8 and 10. She did not experience pulmonary or graft complications in the immediate postoperative period. Four months post-transplant standard dosing ETI was restarted. Despite frequent tacrolimus dose adjustments due to trough fluctuations, she exhibited improvements in FEV1 from 32% to 79% and gained ~30 kg in weight. One year following transplantation, she demonstrates appropriate liver and stable pulmonary function, experiencing only one episode of presumed acute cellular rejection, though the pathological examination was nonspecific.
Discussion: Liver transplant alone in patients with CF is a challenging decision due to unknown outcomes and potential drug-drug interactions between CFTR modulators and post-transplant immunosuppressive regimens; however, this can be considered in CF patients without a prohibitive pulmonary risk and with a previous positive response to modulators. A proactive approach to monitoring tacrolimus troughs and ETI doses after transplant must be carefully planned.
Disclosures:
Richard Maradiaga, MD1, Mitchell Ramsey, MD2, Lindsay A. Sobotka, DO2. P1117 - The Role of CFTR Modulators After Liver Transplantation in Patients with Cystic Fibrosis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Ohio State University Wexner Medical Center, Columbus, OH; 2The Ohio State Wexner Medical Center, Columbus, OH
Introduction: Cystic Fibrosis Transmembrane Conductance Regulator (CFTR) modulators have improved pulmonary outcomes for persons with cystic fibrosis (PwCF). Gastrointestinal manifestations of CF, including cystic fibrosis-related liver disease (CFRLD), are becoming a leading cause of morbidity and mortality in patients with CF—however, the use of CFTR modulators in decompensated cirrhosis and after liver transplantation has not been determined. We present a PwCF who underwent liver transplantation and safely resumed CFTR modulator afterward.
Case Description/Methods: A 22-year-old female with CF (F508del/F508del) complicated by mild CFRLD commenced elexacaftor/tezacaftor/ivacaftor (ETI) at standard dosing and experienced improved pulmonary function. However, her CFRLD progressed over time, and she developed ascites which was managed with diuretics and discontinuation of ETI. Unfortunately, her forced expiratory volume (FEV1) decreased from 54% to 45%, and she endured multiple hospitalizations due to pulmonary exacerbations. Her CFRLD continued to decompensate, developing hepatorenal syndrome requiring intermittent hemodialysis. Her MELD-Na score acutely increased to 40. Our multi-disciplinary transplant committee reviewed her case and jointly agreed to proceed with liver transplantation alone, anticipating improved pulmonary function upon future ETI reinstatement.
Her post-transplant immunosuppression included steroid induction, Cellcept, and tacrolimus with a goal trough between 8 and 10. She did not experience pulmonary or graft complications in the immediate postoperative period. Four months post-transplant standard dosing ETI was restarted. Despite frequent tacrolimus dose adjustments due to trough fluctuations, she exhibited improvements in FEV1 from 32% to 79% and gained ~30 kg in weight. One year following transplantation, she demonstrates appropriate liver and stable pulmonary function, experiencing only one episode of presumed acute cellular rejection, though the pathological examination was nonspecific.
Discussion: Liver transplant alone in patients with CF is a challenging decision due to unknown outcomes and potential drug-drug interactions between CFTR modulators and post-transplant immunosuppressive regimens; however, this can be considered in CF patients without a prohibitive pulmonary risk and with a previous positive response to modulators. A proactive approach to monitoring tacrolimus troughs and ETI doses after transplant must be carefully planned.
Disclosures:
Richard Maradiaga indicated no relevant financial relationships.
Mitchell Ramsey indicated no relevant financial relationships.
Lindsay Sobotka indicated no relevant financial relationships.
Richard Maradiaga, MD1, Mitchell Ramsey, MD2, Lindsay A. Sobotka, DO2. P1117 - The Role of CFTR Modulators After Liver Transplantation in Patients with Cystic Fibrosis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
