Sunday Poster Session
Category: Liver
P1122 - Obstructive Jaundice: Lurking Between Two Zebras
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Matthew Reif, MD
Tulane University
New Orleans, LA
Presenting Author(s)
Matthew Reif, MD1, Eric Lorio, MD2, Victoria Jackson, MD1, Gary M. Reiss, MD1, Peng-Sheng Ting, MD1
1Tulane University, New Orleans, LA; 2Tulane University School of Medicine, New Orleans, LA
Introduction: Obstructive jaundice in young patients generally prompts a focused differential based on distal biliary obstruction, but proximal obstructions require a more extensive workup. Here, we present a perplexing case of proximal biliary obstruction in a young male.
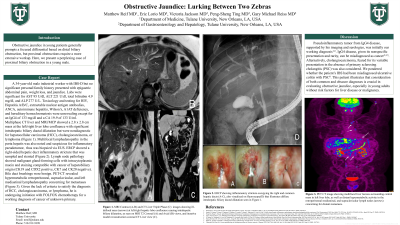
Case Description/Methods: A 34-year-old male industrial worker with IBS-D but no significant personal/family history presented with epigastric abdominal pain, weight loss, and jaundice. Labs were significant for AST 95 U/dl, ALT 221 U/dl, Total bilirubin 4.9 mg/dl, and ALP 277 U/L. Toxicology and testing for HIV, Hepatitis A/B/C, extractable nuclear antigen antibodies, ANCA, autoimmune hepatitis, Wilson’s, A1AT deficiency, and hereditary hemochromatosis were unrevealing except for an IgG4 of 133 mg/dl and a CA 19-9 of 133 U/ml. Phase CT liver and MRI showed a 2.8 x 2.8 cm mass at the left/right liver lobe confluence with significant intrahepatic biliary ductal dilatation but were nondiagnostic for hepatocellular carcinoma (HCC), cholangiocarcinoma, or lymphoma (Fig 1). Multifocal lymphadenopathy in the porta hepatis was also noted and suspicious for inflammatory pseudotumor. ERCP showed a right-sided hepatic duct inflammatory stricture that was sampled and stented (Fig 2). Lymph node pathology showed malignant gland-forming cells with intracytoplasmic mucin and staining compatible with cancer of hepatobiliary origin (CK19 and CDX2 positive, CK7 and CK20 negative). Bile duct brushings were benign. PET-CT revealed hypermetabolic retroperitoneal, supraclavicular, and left mediastinal lymphadenopathy concerning for metastases (Fig 3). Given the lack of criteria to satisfy the diagnosis of HCC, cholangiocarcinoma, or lymphoma, he is undergoing initiation with FOLFOX chemotherapy for a working diagnosis of cancer of unknown primary.
Discussion: Pseudoinflammatory tumor from IgG4 disease, supported by his imaging and serologies, was initially our working diagnosis1-6. IgG4 disease, given its nonspecific presentation and rarity, is misdiagnosed as cancer2,3,5. Alternatively, cholangiocarcinoma, feared for its variable presentation in the absence of primary sclerosing cholangitis (PSC), was also considered. We pondered whether the patient’s IBS had been misdiagnosed ulcerative colitis with PSC8. This patient illustrates that consideration of both common and obscure diagnoses is crucial in evaluating obstructive jaundice, especially in young adults without risk factors for liver disease or malignancy.

Disclosures:
Matthew Reif, MD1, Eric Lorio, MD2, Victoria Jackson, MD1, Gary M. Reiss, MD1, Peng-Sheng Ting, MD1. P1122 - Obstructive Jaundice: Lurking Between Two Zebras, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Tulane University, New Orleans, LA; 2Tulane University School of Medicine, New Orleans, LA
Introduction: Obstructive jaundice in young patients generally prompts a focused differential based on distal biliary obstruction, but proximal obstructions require a more extensive workup. Here, we present a perplexing case of proximal biliary obstruction in a young male.
Case Description/Methods: A 34-year-old male industrial worker with IBS-D but no significant personal/family history presented with epigastric abdominal pain, weight loss, and jaundice. Labs were significant for AST 95 U/dl, ALT 221 U/dl, Total bilirubin 4.9 mg/dl, and ALP 277 U/L. Toxicology and testing for HIV, Hepatitis A/B/C, extractable nuclear antigen antibodies, ANCA, autoimmune hepatitis, Wilson’s, A1AT deficiency, and hereditary hemochromatosis were unrevealing except for an IgG4 of 133 mg/dl and a CA 19-9 of 133 U/ml. Phase CT liver and MRI showed a 2.8 x 2.8 cm mass at the left/right liver lobe confluence with significant intrahepatic biliary ductal dilatation but were nondiagnostic for hepatocellular carcinoma (HCC), cholangiocarcinoma, or lymphoma (Fig 1). Multifocal lymphadenopathy in the porta hepatis was also noted and suspicious for inflammatory pseudotumor. ERCP showed a right-sided hepatic duct inflammatory stricture that was sampled and stented (Fig 2). Lymph node pathology showed malignant gland-forming cells with intracytoplasmic mucin and staining compatible with cancer of hepatobiliary origin (CK19 and CDX2 positive, CK7 and CK20 negative). Bile duct brushings were benign. PET-CT revealed hypermetabolic retroperitoneal, supraclavicular, and left mediastinal lymphadenopathy concerning for metastases (Fig 3). Given the lack of criteria to satisfy the diagnosis of HCC, cholangiocarcinoma, or lymphoma, he is undergoing initiation with FOLFOX chemotherapy for a working diagnosis of cancer of unknown primary.
Discussion: Pseudoinflammatory tumor from IgG4 disease, supported by his imaging and serologies, was initially our working diagnosis1-6. IgG4 disease, given its nonspecific presentation and rarity, is misdiagnosed as cancer2,3,5. Alternatively, cholangiocarcinoma, feared for its variable presentation in the absence of primary sclerosing cholangitis (PSC), was also considered. We pondered whether the patient’s IBS had been misdiagnosed ulcerative colitis with PSC8. This patient illustrates that consideration of both common and obscure diagnoses is crucial in evaluating obstructive jaundice, especially in young adults without risk factors for liver disease or malignancy.

Figure: Figure 1. MRI Contrast (A-B) CT Liver Triple Phase (C) Images showing ill-defined mass (arrows) at left/right hepatic lobe confluence causing intrahepatic biliary dilatation, as seen on MRI T2 Coronal (A) and Axial (B) views, and iterative model reconstruction coronal CT Liver view (C).
Figure 2. ERCP showing inflammatory stricture occupying right and common hepatic duct (A-C), also visualized on fluoroscopy(D).
Figure 3. PET CT image showing multifocal liver lesions surrounding central mass in left liver lobe, as well as distant hypermetabolic activity in the retroperitoneal mediastinal, and supraclavicular lymph nodes (arrows) concerning for distant metastasis.
Figure 2. ERCP showing inflammatory stricture occupying right and common hepatic duct (A-C), also visualized on fluoroscopy(D).
Figure 3. PET CT image showing multifocal liver lesions surrounding central mass in left liver lobe, as well as distant hypermetabolic activity in the retroperitoneal mediastinal, and supraclavicular lymph nodes (arrows) concerning for distant metastasis.
Disclosures:
Matthew Reif indicated no relevant financial relationships.
Eric Lorio indicated no relevant financial relationships.
Victoria Jackson indicated no relevant financial relationships.
Gary Reiss indicated no relevant financial relationships.
Peng-Sheng Ting indicated no relevant financial relationships.
Matthew Reif, MD1, Eric Lorio, MD2, Victoria Jackson, MD1, Gary M. Reiss, MD1, Peng-Sheng Ting, MD1. P1122 - Obstructive Jaundice: Lurking Between Two Zebras, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
