Sunday Poster Session
Category: Liver
P1130 - Aggressive Tumor Recurrence After Transarterial Chemoembolization for Hepatocellular Carcinoma: A Case Series
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Aishwarya Thakurdesai, MBBS, MD
University of Louisville School of Medicine
Louisville, KY
Presenting Author(s)
Aishwarya Thakurdesai, MBBS, MD, Sohail Contractor, MD, Loretta Jophlin, MD, PhD, Dylan Adamson, MD, Ashutosh J. Barve, MD, PhD
University of Louisville School of Medicine, Louisville, KY
Introduction: Transarterial chemoembolization (TACE) is a minimally invasive procedure combining local chemotherapy administration with hepatic arterial embolization to treat hepatocellular carcinoma (HCC). Multiple studies have proven TACE to prolong survival in HCC patients. It is the current standard of care for unresectable intrahepatic tumors with no vascular invasion or distant metastasis. Rapid intrahepatic tumor progression following TACE is rare. Here, we report 2 cases of aggressive recurrence of HCC following TACE.
Case Description/Methods: Case 1: 66-year-old female with hepatitis C cirrhosis was noted to have serial elevations in Alfa-fetoprotein (AFP). MRI showed a 2.8 cm lesion in the caudate lobe of the liver with arterial enhancement. TACE followed by microwave ablation was performed. Post-TACE MRI was read as showing hepatic infarction, but no active HCC. Over the next 6 weeks, patient developed increasing abdominal pain and worsening liver function tests (LFTs). CT and MRI revealed a large (10.9 cm), irregular hepatic mass with arterial enhancement and washout (LR-5) and extensive thrombus in the portal veins (LRT-IV). Biopsy confirmed HCC. Thus, the patient now had advanced HCC with macrovascular spread. Systemic chemotherapy, her only treatment option, was started. She is currently doing well on it.
Case 2: 52-year-old male with alcoholic cirrhosis was found to have a 3.7 cm right hepatic lesion with arterial enhancement and venous washout (LR-5) on surveillance MRI. A biopsy confirmed HCC, and he underwent TACE. Post-TACE CT showed no suspicious lesions. Three months later, he was hospitalized for abdominal pain. MRI showed a 7.5 cm tumor within the right hepatic lobe (LR-5), with a large extrahepatic soft tissue mass (4.1 cm x 11.3 cm) contiguous with the tumor and abutting the diaphragm. Tumor thrombus was seen in the right hepatic vein (LRT-IV). Systemic chemotherapy was initiated, being the only option. The patient unfortunately passed away a month later due to respiratory failure from pneumonia.
Discussion: Aggressive recurrence of HCC following TACE is a challenging and intriguing occurrence. Mechanisms proposed to explain this include an increase in hypoxia-inducible factor-1 which promotes tumor breakthrough and angiogenesis in response to hypoxia caused by TACE. Aggressive recurrence after combined TACE and radiofrequency ablation (RFA) for HCCs has been found to be very low. Combining TACE with antiangiogenic agents and/or RFA may help combat this life-threatening complication.

Disclosures:
Aishwarya Thakurdesai, MBBS, MD, Sohail Contractor, MD, Loretta Jophlin, MD, PhD, Dylan Adamson, MD, Ashutosh J. Barve, MD, PhD. P1130 - Aggressive Tumor Recurrence After Transarterial Chemoembolization for Hepatocellular Carcinoma: A Case Series, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
University of Louisville School of Medicine, Louisville, KY
Introduction: Transarterial chemoembolization (TACE) is a minimally invasive procedure combining local chemotherapy administration with hepatic arterial embolization to treat hepatocellular carcinoma (HCC). Multiple studies have proven TACE to prolong survival in HCC patients. It is the current standard of care for unresectable intrahepatic tumors with no vascular invasion or distant metastasis. Rapid intrahepatic tumor progression following TACE is rare. Here, we report 2 cases of aggressive recurrence of HCC following TACE.
Case Description/Methods: Case 1: 66-year-old female with hepatitis C cirrhosis was noted to have serial elevations in Alfa-fetoprotein (AFP). MRI showed a 2.8 cm lesion in the caudate lobe of the liver with arterial enhancement. TACE followed by microwave ablation was performed. Post-TACE MRI was read as showing hepatic infarction, but no active HCC. Over the next 6 weeks, patient developed increasing abdominal pain and worsening liver function tests (LFTs). CT and MRI revealed a large (10.9 cm), irregular hepatic mass with arterial enhancement and washout (LR-5) and extensive thrombus in the portal veins (LRT-IV). Biopsy confirmed HCC. Thus, the patient now had advanced HCC with macrovascular spread. Systemic chemotherapy, her only treatment option, was started. She is currently doing well on it.
Case 2: 52-year-old male with alcoholic cirrhosis was found to have a 3.7 cm right hepatic lesion with arterial enhancement and venous washout (LR-5) on surveillance MRI. A biopsy confirmed HCC, and he underwent TACE. Post-TACE CT showed no suspicious lesions. Three months later, he was hospitalized for abdominal pain. MRI showed a 7.5 cm tumor within the right hepatic lobe (LR-5), with a large extrahepatic soft tissue mass (4.1 cm x 11.3 cm) contiguous with the tumor and abutting the diaphragm. Tumor thrombus was seen in the right hepatic vein (LRT-IV). Systemic chemotherapy was initiated, being the only option. The patient unfortunately passed away a month later due to respiratory failure from pneumonia.
Discussion: Aggressive recurrence of HCC following TACE is a challenging and intriguing occurrence. Mechanisms proposed to explain this include an increase in hypoxia-inducible factor-1 which promotes tumor breakthrough and angiogenesis in response to hypoxia caused by TACE. Aggressive recurrence after combined TACE and radiofrequency ablation (RFA) for HCCs has been found to be very low. Combining TACE with antiangiogenic agents and/or RFA may help combat this life-threatening complication.

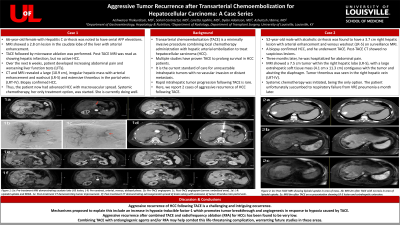
Figure: (A) Case 1: MRI scan prior to TACE demonstrating initial lesion in the caudate lobe of the liver with arterial enhancement (red arrow)
(B) Case 1: MRI scan post-TACE demonstrating new, irregular hepatic mass with arterial enhancement and portal venous extension (red arrow)
(C) Case 2: CT scan post-TACE demonstrating site of initial right hepatic lobe lesion treated by TACE with retained lipoidol (red arrow). No other suspicious lesions seen.
(D) Case 2: MRI scan post-TACE demonstrating new tumor with arterial enhancement in the right hepatic lobe (red arrow) with extrahepatic extension, not present on prior CT scan.
(B) Case 1: MRI scan post-TACE demonstrating new, irregular hepatic mass with arterial enhancement and portal venous extension (red arrow)
(C) Case 2: CT scan post-TACE demonstrating site of initial right hepatic lobe lesion treated by TACE with retained lipoidol (red arrow). No other suspicious lesions seen.
(D) Case 2: MRI scan post-TACE demonstrating new tumor with arterial enhancement in the right hepatic lobe (red arrow) with extrahepatic extension, not present on prior CT scan.
Disclosures:
Aishwarya Thakurdesai indicated no relevant financial relationships.
Sohail Contractor indicated no relevant financial relationships.
Loretta Jophlin indicated no relevant financial relationships.
Dylan Adamson indicated no relevant financial relationships.
Ashutosh Barve indicated no relevant financial relationships.
Aishwarya Thakurdesai, MBBS, MD, Sohail Contractor, MD, Loretta Jophlin, MD, PhD, Dylan Adamson, MD, Ashutosh J. Barve, MD, PhD. P1130 - Aggressive Tumor Recurrence After Transarterial Chemoembolization for Hepatocellular Carcinoma: A Case Series, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
