Sunday Poster Session
Category: Liver
P1133 - Portal Hypertension and Cirrhosis Unveiled: An Unexpected Finding of a Visceral Venous Aneurysm
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Jessica Sosio, DO
Indiana University
Evansville, IN
Presenting Author(s)
Jessica Sosio, DO1, Colin Martyn, MD1, Margaret Beliveau-Ficalora, MD1, Oluwagbenga Serrano, FACG2
1Indiana University, Evansville, IN; 2Indiana University, Vincennes, IN
Introduction: Deep visceral venous aneurysms are exceedingly rare compared to arterial aneurysms. Most venous aneurysms are superficial and located in the popliteal, jugular, or saphenous veins, but about 3% involve deeper visceral veins such as those of the portal venous system. These aneurysms are often discovered incidentally but can present with various clinical manifestations such as vague abdominal pain. We present the case of an 81-year-old man found to have an incidental 3.8 cm superior mesenteric vein (SMV) aneurysm and portal hypertension (PHT) during surveillance of a postoperative scrotal hematoma.
Case Description/Methods: Our patient is an 81-year-old man with a history of atrial fibrillation and radical right nephrectomy for renal cell carcinoma who presented in clinic 5 months after a laparoscopic bilateral inguinal herniorrhaphy. Serial abdominal CTs had been obtained to monitor the resolution of a postoperative scrotal hematoma. His initial CT 2 weeks after herniorrhaphy revealed an incidental 3.8 cm SMV aneurysm without other pathology, but a subsequent CT 4 months later discovered new-onset large volume ascites, cirrhosis, and splenomegaly without an increase in SMV aneurysm dimensions. These abnormal findings persisted without change on an abdominal MRI with contrast 6 months postoperatively. Our patient denied alcohol use, abdominal pain, nausea, jaundice, and change in stool frequency or color. Vitals were within normal limits and physical examination demonstrated peripheral edema. Despite extensive evaluation, no obvious etiology for his new cirrhosis was found. Additionally, a remote abdominal CT 9 years prior to the herniorrhaphy did not demonstrate either cirrhosis or an SMV aneurysm.
Discussion: Visceral venous aneurysms can form secondary to PHT, pancreatitis, trauma, and surgery. Our patient had undergone laparoscopic surgery which can increase the risk of venous aneurysm development via splanchnic vasodilation when PHT is present. The cause of his cirrhosis remained undetermined, but potential etiologies include underlying NASH or medication induced liver injury. Aneurysms of portal venous structures are typically benign warranting only surveillance imaging, but intervention may be required in cases of portal venous thrombosis, venous rupture, or locoregional compression from aneurysmal dilatation. Given the absence of complications in our patient, an annual surveillance protocol with abdominal MRI was recommended.

Disclosures:
Jessica Sosio, DO1, Colin Martyn, MD1, Margaret Beliveau-Ficalora, MD1, Oluwagbenga Serrano, FACG2. P1133 - Portal Hypertension and Cirrhosis Unveiled: An Unexpected Finding of a Visceral Venous Aneurysm, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Indiana University, Evansville, IN; 2Indiana University, Vincennes, IN
Introduction: Deep visceral venous aneurysms are exceedingly rare compared to arterial aneurysms. Most venous aneurysms are superficial and located in the popliteal, jugular, or saphenous veins, but about 3% involve deeper visceral veins such as those of the portal venous system. These aneurysms are often discovered incidentally but can present with various clinical manifestations such as vague abdominal pain. We present the case of an 81-year-old man found to have an incidental 3.8 cm superior mesenteric vein (SMV) aneurysm and portal hypertension (PHT) during surveillance of a postoperative scrotal hematoma.
Case Description/Methods: Our patient is an 81-year-old man with a history of atrial fibrillation and radical right nephrectomy for renal cell carcinoma who presented in clinic 5 months after a laparoscopic bilateral inguinal herniorrhaphy. Serial abdominal CTs had been obtained to monitor the resolution of a postoperative scrotal hematoma. His initial CT 2 weeks after herniorrhaphy revealed an incidental 3.8 cm SMV aneurysm without other pathology, but a subsequent CT 4 months later discovered new-onset large volume ascites, cirrhosis, and splenomegaly without an increase in SMV aneurysm dimensions. These abnormal findings persisted without change on an abdominal MRI with contrast 6 months postoperatively. Our patient denied alcohol use, abdominal pain, nausea, jaundice, and change in stool frequency or color. Vitals were within normal limits and physical examination demonstrated peripheral edema. Despite extensive evaluation, no obvious etiology for his new cirrhosis was found. Additionally, a remote abdominal CT 9 years prior to the herniorrhaphy did not demonstrate either cirrhosis or an SMV aneurysm.
Discussion: Visceral venous aneurysms can form secondary to PHT, pancreatitis, trauma, and surgery. Our patient had undergone laparoscopic surgery which can increase the risk of venous aneurysm development via splanchnic vasodilation when PHT is present. The cause of his cirrhosis remained undetermined, but potential etiologies include underlying NASH or medication induced liver injury. Aneurysms of portal venous structures are typically benign warranting only surveillance imaging, but intervention may be required in cases of portal venous thrombosis, venous rupture, or locoregional compression from aneurysmal dilatation. Given the absence of complications in our patient, an annual surveillance protocol with abdominal MRI was recommended.

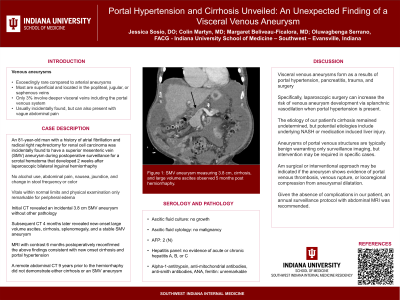
Figure: Figure 1: SMV aneurysm measuring 3.8 cm, cirrhosis, and large volume ascites observed 5 months post herniorrhaphy.
Disclosures:
Jessica Sosio indicated no relevant financial relationships.
Colin Martyn indicated no relevant financial relationships.
Margaret Beliveau-Ficalora indicated no relevant financial relationships.
Oluwagbenga Serrano indicated no relevant financial relationships.
Jessica Sosio, DO1, Colin Martyn, MD1, Margaret Beliveau-Ficalora, MD1, Oluwagbenga Serrano, FACG2. P1133 - Portal Hypertension and Cirrhosis Unveiled: An Unexpected Finding of a Visceral Venous Aneurysm, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
