Sunday Poster Session
Category: Liver
P1138 - Flood Syndrome: A Case Report With Discussion on Optimal Treatments
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio
- JS
Jowana Saba, MD
Tulane University School of Medicine
New Orleans, Louisiana
Presenting Author(s)
Jowana Saba, MD1, Jaya Bommireddipally, MD2, Justin Roy, MD1, Benjamin A. Guider, MD1
1Tulane University School of Medicine, New Orleans, LA; 2Tulane University, New Orleans, LA
Introduction: The most common initial manifestation of decompensated cirrhosis is ascites. 5-10% of patients with cirrhosis will develop ascites per year resulting in reduction of the 5-year survival from 80% to 30%. 20% of patients with cirrhosis develop umbilical hernia. Spontaneous rupture of the umbilical hernia was first described by Johnson in 1901 and became known as Flood Syndrome in 1961 after Frank Flood. It corresponds to a rush of ascitic fluid through a skin lesion and can be complicated by large-volume paracentesis with subsequent hypotension, evisceration, bowel incarceration, and peritonitis with a 30% morbidity and mortality rate.
Case Description/Methods: A 56-year-old man with NASH cirrhosis (Child-Pugh B, MELD 12) complicated by esophageal varices, ascites, and an umbilical hernia presented with a ruptured umbilical hernia that had profusely discharged fluid for approximately 10 minutes. On presentation, he was hemodynamically stable. Abdominal exam showed a mildly distended abdomen with lower quadrant tenderness and an umbilical hernia draining straw-colored fluid. Computerized tomography (CT) abdomen showed ascites containing a ventral hernia with inflammatory changes in the subcutaneous tissue within and surrounding the hernia. He was treated with albumin for large-volume paracentesis, ceftriaxone given the communication of the peritoneal cavity with the environment, furosemide and spironolactone for optimal ascites control followed by hernia repair with appropriate recovery.
Discussion: There is no clear recommendation for the treatment of a ruptured umbilical hernia. Urgent surgical repair results in 6-20% mortality, versus 60-80% with conservative management alone. The most important point is to initiate conservative therapy prior to the surgery which includes patient evaluation, hemodynamic stabilization, optimal ascites control, wound care, antibiotics, and correction of coagulopathies, thrombocytopenia, and electrolytes. The timing of the surgical treatment is debatable, and the duration of optimal conservative management is lacking. Emergent surgical repair prior to optimization increases the chances of wound dehiscence and evisceration. Patients who are not surgical candidates or refuse surgery can be treated with fibrin-based glue injection in the defect or with a peritoneal pigtail. The optimal ascites control represents the mainstay in the prevention of umbilical hernia occurrence and rupture.

Disclosures:
Jowana Saba, MD1, Jaya Bommireddipally, MD2, Justin Roy, MD1, Benjamin A. Guider, MD1. P1138 - Flood Syndrome: A Case Report With Discussion on Optimal Treatments, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Tulane University School of Medicine, New Orleans, LA; 2Tulane University, New Orleans, LA
Introduction: The most common initial manifestation of decompensated cirrhosis is ascites. 5-10% of patients with cirrhosis will develop ascites per year resulting in reduction of the 5-year survival from 80% to 30%. 20% of patients with cirrhosis develop umbilical hernia. Spontaneous rupture of the umbilical hernia was first described by Johnson in 1901 and became known as Flood Syndrome in 1961 after Frank Flood. It corresponds to a rush of ascitic fluid through a skin lesion and can be complicated by large-volume paracentesis with subsequent hypotension, evisceration, bowel incarceration, and peritonitis with a 30% morbidity and mortality rate.
Case Description/Methods: A 56-year-old man with NASH cirrhosis (Child-Pugh B, MELD 12) complicated by esophageal varices, ascites, and an umbilical hernia presented with a ruptured umbilical hernia that had profusely discharged fluid for approximately 10 minutes. On presentation, he was hemodynamically stable. Abdominal exam showed a mildly distended abdomen with lower quadrant tenderness and an umbilical hernia draining straw-colored fluid. Computerized tomography (CT) abdomen showed ascites containing a ventral hernia with inflammatory changes in the subcutaneous tissue within and surrounding the hernia. He was treated with albumin for large-volume paracentesis, ceftriaxone given the communication of the peritoneal cavity with the environment, furosemide and spironolactone for optimal ascites control followed by hernia repair with appropriate recovery.
Discussion: There is no clear recommendation for the treatment of a ruptured umbilical hernia. Urgent surgical repair results in 6-20% mortality, versus 60-80% with conservative management alone. The most important point is to initiate conservative therapy prior to the surgery which includes patient evaluation, hemodynamic stabilization, optimal ascites control, wound care, antibiotics, and correction of coagulopathies, thrombocytopenia, and electrolytes. The timing of the surgical treatment is debatable, and the duration of optimal conservative management is lacking. Emergent surgical repair prior to optimization increases the chances of wound dehiscence and evisceration. Patients who are not surgical candidates or refuse surgery can be treated with fibrin-based glue injection in the defect or with a peritoneal pigtail. The optimal ascites control represents the mainstay in the prevention of umbilical hernia occurrence and rupture.

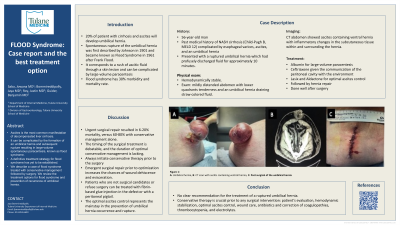
Figure: Figure 1: A: Umbilical hernia.
B: Umbilical hernia.
C: Computerized tomography (CT) abdomen with ascites and a ventral hernia with inflammatory changes in the subcutaneous tissue within and surrounding the hernia.
D: Post-surgical abdominal incision after hernia repair.
B: Umbilical hernia.
C: Computerized tomography (CT) abdomen with ascites and a ventral hernia with inflammatory changes in the subcutaneous tissue within and surrounding the hernia.
D: Post-surgical abdominal incision after hernia repair.
Disclosures:
Jowana Saba indicated no relevant financial relationships.
Jaya Bommireddipally indicated no relevant financial relationships.
Justin Roy indicated no relevant financial relationships.
Benjamin Guider indicated no relevant financial relationships.
Jowana Saba, MD1, Jaya Bommireddipally, MD2, Justin Roy, MD1, Benjamin A. Guider, MD1. P1138 - Flood Syndrome: A Case Report With Discussion on Optimal Treatments, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
