Sunday Poster Session
Category: Liver
P1147 - Significant Neurologic Complications After Transjugular Intrahepatic Portosystemic Shunt for Severe Upper Gastrointestinal Bleed
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Nathan Pham, MD
University of Washington
Seattle, WA
Presenting Author(s)
Nathan Pham, MD, Lei Yu, MD
University of Washington, Seattle, WA
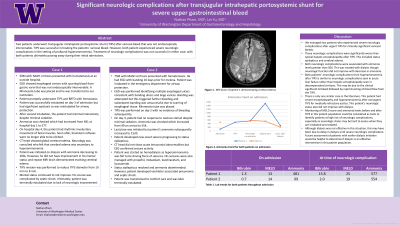
Introduction: Two patients underwent transjugular intrahepatic portosystemic shunt (TIPS) after variceal bleed that was not endoscopically intervenable. After TIPS, both patients experienced severe neurologic complications in the setting of profound hyperammonemia.
Case Description/Methods: Case 1 is a 58-year-old male with NASH cirrhosis presenting with hematemesis. EGD showed esophageal varices with spurting blood from a gastric varix that was not endoscopically intervenable. He then underwent TIPS with hemostasis.
He had minimal interactivity while intubated despite minimal sedation. An ammonia was 577. His neurologic status worsened with loss of brainstem reflexes. CT head identified global cerebral edema which was thought to be from hyperammonemia. He underwent dialysis with ammonia decreasing to below 200. However, his mental status did not improve and repeat imaging showed worsening edema. Patient was later transitioned to comfort care.
Case 2 is a 75-year-old male with NASH cirrhosis who presented with hematemesis. EGD demonstrated large varices and ulcers from recent banding; the varices were unsuccessfully banded due to varices not being adequately suctioned into the banding device. He underwent TIPS with hemostasis.
After TIPS he did not have response to noxious stimuli with no sedation. Ammonia was 554. Lactulose was initiated but mental status did not improve and his ammonia increased to 1520. He then developed status epilepticus requiring multiple antiepileptics. Dialysis was initiated as hyperammonemia was thought to be the cause of his seizures. His seizures resolved with this treatment. However, he went into septic shock and family decided to transition patient to comfort care.
Discussion: We managed two patients who experienced significant neurologic both thought to be in the setting of hyperammonemia after his TIPS. Historically, ammonia is not a diagnostic or prognostic tool used in hepatic encephalopathy for cirrhosis. However, these cases could be considered unusual manifestations of hepatic encephalopathy (HE) as they occurred in the setting of variceal bleed and emergent TIPS in patients without prior history of HE. It is possible that the pathophysiology of these patients’ neurologic complications may be similar to acute liver failure patients, where monitoring ammonia is more vital and neurologic complications are more severe. Future consideration of early dialysis for patients with similar presentations should be considered given the severity of neurologic complications.
Disclosures:
Nathan Pham, MD, Lei Yu, MD. P1147 - Significant Neurologic Complications After Transjugular Intrahepatic Portosystemic Shunt for Severe Upper Gastrointestinal Bleed, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
University of Washington, Seattle, WA
Introduction: Two patients underwent transjugular intrahepatic portosystemic shunt (TIPS) after variceal bleed that was not endoscopically intervenable. After TIPS, both patients experienced severe neurologic complications in the setting of profound hyperammonemia.
Case Description/Methods: Case 1 is a 58-year-old male with NASH cirrhosis presenting with hematemesis. EGD showed esophageal varices with spurting blood from a gastric varix that was not endoscopically intervenable. He then underwent TIPS with hemostasis.
He had minimal interactivity while intubated despite minimal sedation. An ammonia was 577. His neurologic status worsened with loss of brainstem reflexes. CT head identified global cerebral edema which was thought to be from hyperammonemia. He underwent dialysis with ammonia decreasing to below 200. However, his mental status did not improve and repeat imaging showed worsening edema. Patient was later transitioned to comfort care.
Case 2 is a 75-year-old male with NASH cirrhosis who presented with hematemesis. EGD demonstrated large varices and ulcers from recent banding; the varices were unsuccessfully banded due to varices not being adequately suctioned into the banding device. He underwent TIPS with hemostasis.
After TIPS he did not have response to noxious stimuli with no sedation. Ammonia was 554. Lactulose was initiated but mental status did not improve and his ammonia increased to 1520. He then developed status epilepticus requiring multiple antiepileptics. Dialysis was initiated as hyperammonemia was thought to be the cause of his seizures. His seizures resolved with this treatment. However, he went into septic shock and family decided to transition patient to comfort care.
Discussion: We managed two patients who experienced significant neurologic both thought to be in the setting of hyperammonemia after his TIPS. Historically, ammonia is not a diagnostic or prognostic tool used in hepatic encephalopathy for cirrhosis. However, these cases could be considered unusual manifestations of hepatic encephalopathy (HE) as they occurred in the setting of variceal bleed and emergent TIPS in patients without prior history of HE. It is possible that the pathophysiology of these patients’ neurologic complications may be similar to acute liver failure patients, where monitoring ammonia is more vital and neurologic complications are more severe. Future consideration of early dialysis for patients with similar presentations should be considered given the severity of neurologic complications.
Disclosures:
Nathan Pham indicated no relevant financial relationships.
Lei Yu indicated no relevant financial relationships.
Nathan Pham, MD, Lei Yu, MD. P1147 - Significant Neurologic Complications After Transjugular Intrahepatic Portosystemic Shunt for Severe Upper Gastrointestinal Bleed, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
