Sunday Poster Session
Category: Obesity
P1169 - Impact of Obesity on Clinical Outcomes in Patients Hospitalized for Upper Gastrointestinal Bleed in a Community Hospital—A Retrospective Cohort Study
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Mithil Gowda Suresh, MD
Saint Vincent Hospital
Chicopee, MA
Presenting Author(s)
Mithil Gowda Suresh, MD1, Yuvaraj Singh, MD1, Jassimran Singh, MD1, Aakriti soni, MD1, Anuroop Yekula, MD1, Curuchi Anand, MD1, Safia Mohamed, MD2, Maya Gogtay, MD3
1Saint Vincent Hospital, Worcester, MA; 2NYMC/Landmark Medical Center, Woonsocket, MA; 3University of Texas Health, San Antonio, TX
Introduction: Upper Gastrointestinal Bleeding (UGIB) is responsible for 350,000 hospital admissions annually in the United States, often requiring blood transfusions, inpatient gastroenterology consultation, endoscopy and ICU stay, which increases the overall investigation cost of treatment and length of stay. Obese individuals have a higher burden of comorbidities and are on medications like aspirin, apixaban, NSAID thereby increasing the incidence and severity of a UGIB episode. Few studies have explored the impact of obesity on UGIB outcomes.
Methods: Our Institutional Review Board approved this retrospective cohort study. We included all adult patients admitted with a diagnosis of UGIB between 2021-2022. Obesity was characterized as BMI ≥ 30kg/m2. Variables included demographics, vitals, laboratory values, medications, the requirement of blood transfusion, hospitalization days, and readmission rate. Continuous variables were assessed using the independent t-test, and categorical variables using chi-square. p< 0.05 were considered statistically significant.
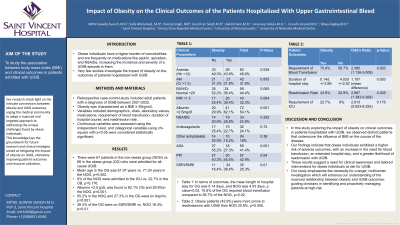
Results: There were 67 patients in the non-obese group (NOG) vs. 66 in the obese group (OG) admitted for all-cause UGIB cohort. Mean age in the OG was 61.97 years vs 71.24 years in the NOG. At the time of hospitalization, 9% of the NOG were admitted to the ICU vs. 22.7% in the OB, p=0.176. Albumin < 2.5 g/dL was found in 62.1% OG and 29.9%in the NOG, p=0.001. 55.2% in the NOG and 27.3% in the OG were on Aspirin, p=0.001. 36.4% of the OG were on SSRI/SNRI vs. NOG 16.4%, p=0.01. Table 1 shows the remaining clinical parameters between the two groups. The mean length of hospital stay for OG was 5.14 days, and NOG was 4.03 days, p value=0.02. 75.8% in OG required blood transfusion compared to 56.7% in NOG, p=0.02. Obese patients were more prone to readmissions than NOG (43.9% vs 20.9%, p=0.005) (Table 2).
Discussion: Obese individuals with UGIB had more blood transfusions, extended hospital stay, and readmissions. Though statistically less significant, a trend towards more ICU admission was noted in the OG. In addition, our study shows that obese patients had a significant increase in resource utilization as compared to non-obese individuals. A large multicenter study to validate the association between obesity and UGIB outcomes is required, focusing on mortality risk. It will help clinicians identify and address the effect of weight on patients at high risk of UGIB and have a targeted approach toward weight reduction.

Disclosures:
Mithil Gowda Suresh, MD1, Yuvaraj Singh, MD1, Jassimran Singh, MD1, Aakriti soni, MD1, Anuroop Yekula, MD1, Curuchi Anand, MD1, Safia Mohamed, MD2, Maya Gogtay, MD3. P1169 - Impact of Obesity on Clinical Outcomes in Patients Hospitalized for Upper Gastrointestinal Bleed in a Community Hospital—A Retrospective Cohort Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Saint Vincent Hospital, Worcester, MA; 2NYMC/Landmark Medical Center, Woonsocket, MA; 3University of Texas Health, San Antonio, TX
Introduction: Upper Gastrointestinal Bleeding (UGIB) is responsible for 350,000 hospital admissions annually in the United States, often requiring blood transfusions, inpatient gastroenterology consultation, endoscopy and ICU stay, which increases the overall investigation cost of treatment and length of stay. Obese individuals have a higher burden of comorbidities and are on medications like aspirin, apixaban, NSAID thereby increasing the incidence and severity of a UGIB episode. Few studies have explored the impact of obesity on UGIB outcomes.
Methods: Our Institutional Review Board approved this retrospective cohort study. We included all adult patients admitted with a diagnosis of UGIB between 2021-2022. Obesity was characterized as BMI ≥ 30kg/m2. Variables included demographics, vitals, laboratory values, medications, the requirement of blood transfusion, hospitalization days, and readmission rate. Continuous variables were assessed using the independent t-test, and categorical variables using chi-square. p< 0.05 were considered statistically significant.
Results: There were 67 patients in the non-obese group (NOG) vs. 66 in the obese group (OG) admitted for all-cause UGIB cohort. Mean age in the OG was 61.97 years vs 71.24 years in the NOG. At the time of hospitalization, 9% of the NOG were admitted to the ICU vs. 22.7% in the OB, p=0.176. Albumin < 2.5 g/dL was found in 62.1% OG and 29.9%in the NOG, p=0.001. 55.2% in the NOG and 27.3% in the OG were on Aspirin, p=0.001. 36.4% of the OG were on SSRI/SNRI vs. NOG 16.4%, p=0.01. Table 1 shows the remaining clinical parameters between the two groups. The mean length of hospital stay for OG was 5.14 days, and NOG was 4.03 days, p value=0.02. 75.8% in OG required blood transfusion compared to 56.7% in NOG, p=0.02. Obese patients were more prone to readmissions than NOG (43.9% vs 20.9%, p=0.005) (Table 2).
Discussion: Obese individuals with UGIB had more blood transfusions, extended hospital stay, and readmissions. Though statistically less significant, a trend towards more ICU admission was noted in the OG. In addition, our study shows that obese patients had a significant increase in resource utilization as compared to non-obese individuals. A large multicenter study to validate the association between obesity and UGIB outcomes is required, focusing on mortality risk. It will help clinicians identify and address the effect of weight on patients at high risk of UGIB and have a targeted approach toward weight reduction.

Figure: Table 1 and 2
Disclosures:
Mithil Gowda Suresh indicated no relevant financial relationships.
Yuvaraj Singh indicated no relevant financial relationships.
Jassimran Singh indicated no relevant financial relationships.
Aakriti soni indicated no relevant financial relationships.
Anuroop Yekula indicated no relevant financial relationships.
Curuchi Anand: Abbvie – Speakers Bureau.
Safia Mohamed indicated no relevant financial relationships.
Maya Gogtay indicated no relevant financial relationships.
Mithil Gowda Suresh, MD1, Yuvaraj Singh, MD1, Jassimran Singh, MD1, Aakriti soni, MD1, Anuroop Yekula, MD1, Curuchi Anand, MD1, Safia Mohamed, MD2, Maya Gogtay, MD3. P1169 - Impact of Obesity on Clinical Outcomes in Patients Hospitalized for Upper Gastrointestinal Bleed in a Community Hospital—A Retrospective Cohort Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
