Sunday Poster Session
Category: Obesity
P1172 - Weight Loss at a Price: Tirzepatide-induced Pneumatosis Intestinalis
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall

Sindhura Kolli, MD
Staten Island University Hospital, Northwell Health
Staten Island, NY
Presenting Author(s)
Sindhura Kolli, MD, Dhineshreddy Gurala, MD, Jean Chalhoub, MD, Sherif Andrawes, MD
Staten Island University Hospital, Northwell Health, Staten Island, NY
Introduction: Tirzepatide is a dual gastric inhibitory peptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist (RA) used off-label for weight loss. Its GLP-1 activity decreases gastric emptying (GE) causing satiety but can increase colonic stool burden. Unchecked, our patient presented with the first reported case of tirzepatide-induced pneumatosis intestinalis (PI).
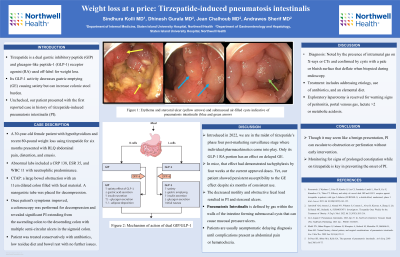
Case Description/Methods: A 30-year-old female patient with hypothyroidism and recent 80 pound weight loss using tirzepatide for six months presented with RLQ abdominal pain, distention, and emesis. Abnormal labs included a CRP 138, ESR 35, and WBC 11 with neutrophilic predominance. Computed tomography (CT) abdomen showed a large bowel obstruction with an 11cm dilated colon filled with fecal material. A nasogastric tube was placed for decompression. Once patient's symptoms improved, a colonoscopy was performed for decompression and revealed significant PI extending from the ascending colon to the descending colon with multiple semi-circular ulcers in the sigmoid colon. Patient was treated conservatively with antibiotics, bowel rest, low residue diet with no further issues.
Discussion: Introduced in 2022, we are in the midst of tirzepatide’s phase four post-marketing surveillance stage where individual pharmacokinetics come into play. Only its GLP-1 RA portion has an effect on delayed GE. In mice, that effect had demonstrated tachyphylaxis by four weeks at the current approved doses. Yet, our patient showed persistent susceptibility to the GE effect despite six months of consistent use. The decreased motility and obstructive fecal load resulted in PI and stercoral ulcers. PI is defined by gas within the walls of the intestine forming submucosal cysts that can cause mucosal pressure ulcers. Patients present asymptomatically delaying diagnosis until complications present as abdominal pain or hematochezia. PI is diagnosed by the presence of intramural gas on XR or CTs, and confirmed endoscopically by the presence of cysts with a pale or bluish surface that deflate when biopsied.Treatment includes addressing etiology, use of antibiotics, and an elemental diet. Exploratory laparotomy is reserved for warning signs of peritonitis, portal venous gas, lactate >2 or metabolic acidosis. Though it may seem like a benign presentation, PI can escalate to obstruction or perforation without early intervention. Monitoring for signs of prolonged constipation while on tirzepatide is key in preventing the onset of PI.

Disclosures:
Sindhura Kolli, MD, Dhineshreddy Gurala, MD, Jean Chalhoub, MD, Sherif Andrawes, MD. P1172 - Weight Loss at a Price: Tirzepatide-induced Pneumatosis Intestinalis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Staten Island University Hospital, Northwell Health, Staten Island, NY
Introduction: Tirzepatide is a dual gastric inhibitory peptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist (RA) used off-label for weight loss. Its GLP-1 activity decreases gastric emptying (GE) causing satiety but can increase colonic stool burden. Unchecked, our patient presented with the first reported case of tirzepatide-induced pneumatosis intestinalis (PI).
Case Description/Methods: A 30-year-old female patient with hypothyroidism and recent 80 pound weight loss using tirzepatide for six months presented with RLQ abdominal pain, distention, and emesis. Abnormal labs included a CRP 138, ESR 35, and WBC 11 with neutrophilic predominance. Computed tomography (CT) abdomen showed a large bowel obstruction with an 11cm dilated colon filled with fecal material. A nasogastric tube was placed for decompression. Once patient's symptoms improved, a colonoscopy was performed for decompression and revealed significant PI extending from the ascending colon to the descending colon with multiple semi-circular ulcers in the sigmoid colon. Patient was treated conservatively with antibiotics, bowel rest, low residue diet with no further issues.
Discussion: Introduced in 2022, we are in the midst of tirzepatide’s phase four post-marketing surveillance stage where individual pharmacokinetics come into play. Only its GLP-1 RA portion has an effect on delayed GE. In mice, that effect had demonstrated tachyphylaxis by four weeks at the current approved doses. Yet, our patient showed persistent susceptibility to the GE effect despite six months of consistent use. The decreased motility and obstructive fecal load resulted in PI and stercoral ulcers. PI is defined by gas within the walls of the intestine forming submucosal cysts that can cause mucosal pressure ulcers. Patients present asymptomatically delaying diagnosis until complications present as abdominal pain or hematochezia. PI is diagnosed by the presence of intramural gas on XR or CTs, and confirmed endoscopically by the presence of cysts with a pale or bluish surface that deflate when biopsied.Treatment includes addressing etiology, use of antibiotics, and an elemental diet. Exploratory laparotomy is reserved for warning signs of peritonitis, portal venous gas, lactate >2 or metabolic acidosis. Though it may seem like a benign presentation, PI can escalate to obstruction or perforation without early intervention. Monitoring for signs of prolonged constipation while on tirzepatide is key in preventing the onset of PI.

Figure: Figure 1: Erythema and stercoral ulcer (yellow arrows) and submucosal air-filled cysts indicative of pneumatosis intestinalis (blue and green arrows)
Disclosures:
Sindhura Kolli indicated no relevant financial relationships.
Dhineshreddy Gurala indicated no relevant financial relationships.
Jean Chalhoub indicated no relevant financial relationships.
Sherif Andrawes indicated no relevant financial relationships.
Sindhura Kolli, MD, Dhineshreddy Gurala, MD, Jean Chalhoub, MD, Sherif Andrawes, MD. P1172 - Weight Loss at a Price: Tirzepatide-induced Pneumatosis Intestinalis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
