Sunday Poster Session
Category: Practice Management
P1221 - Improving Identification of Social Determinants and Equity in Gastroenterology Adverse Events
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Michelle L. Hughes, MD
Yale School of Medicine
New Haven, CT
Presenting Author(s)
Michelle L. Hughes, MD1, Carolyn Haight, MSN, RN, CPHQ2, Aldo Peixoto, MD1, Linda Fan, MD3
1Yale School of Medicine, New Haven, CT; 2Yale New Haven Hospital, New Haven, CT; 3Yale School of Medicine, Guilford, CT
Introduction: Social determinants of health (SDOH) and bias play a role in disease states and outcomes in Gastroenterology (GI) and Hepatology. However, there has been little evaluation on their impact on adverse events or errors within the field and even less guidance on how to incorporate assessment of these factors into event reviews and implementation of change.
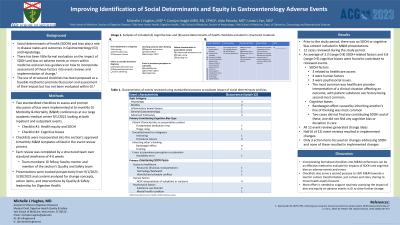
Methods: Two standardized checklists to assess and prompt discussion of bias were implemented at bi-monthly GI Morbidity & Mortality (M&M) conferences at our large academic medical center 9/1/2021. One checklist focused on health equity and SDOH and the second on cognitive biases. Both were incorporated into the section’s approved M&M templates utilized in the event review process. Each review was completed by a structured team of a GI fellow, faculty mentor and member of the section’s Quality and Safety team as per section standard. Presentations were tracked prospectively from 9/1/2021-5/30/2023 and content analyzed.
Results: Prior to the study period, there was no SDOH or cognitive bias content included in M&M presentations. A total of 12 presentations occurred during the study period. An average of 3.3 (range 0-8) SDOH-related factors and 3.8 (range 0-9) cognitive biases were found to contribute to reviewed events. Of the SDOH factors, 3 related to healthcare access, 4 were human factors, and 3 were psychosocial issues. The most common was healthcare provider interpretation of a clinical situation affecting an outcome, with patient substance use history being second most common. Of the cognitive biases, bandwagon effect caused by inheriting another’s line of thinking was most common. Two cases did not find any contributing SDOH and of these, one did not find any cognitive bias or deviation in care. All 12 presentations generated change ideas and 6 resulted in implemented changes. Only 3 action items focused on changes addressing SDOH and none of these resulted in implemented changes.
Discussion: Incorporating formalized checklists into M&M conferences can be an effective method to evaluate for impacts of SDOH and cognitive bias on adverse events and errors in a standardized and meaningful way. They also serve a second purpose to shift M&M towards a tool for culture transformation, just culture and story sharing to move health equity forward. More effort is needed to support routinely assessing the impact of bias and equity on adverse events in Gastroenterology to drive further change.
Disclosures:
Michelle L. Hughes, MD1, Carolyn Haight, MSN, RN, CPHQ2, Aldo Peixoto, MD1, Linda Fan, MD3. P1221 - Improving Identification of Social Determinants and Equity in Gastroenterology Adverse Events, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Yale School of Medicine, New Haven, CT; 2Yale New Haven Hospital, New Haven, CT; 3Yale School of Medicine, Guilford, CT
Introduction: Social determinants of health (SDOH) and bias play a role in disease states and outcomes in Gastroenterology (GI) and Hepatology. However, there has been little evaluation on their impact on adverse events or errors within the field and even less guidance on how to incorporate assessment of these factors into event reviews and implementation of change.
Methods: Two standardized checklists to assess and prompt discussion of bias were implemented at bi-monthly GI Morbidity & Mortality (M&M) conferences at our large academic medical center 9/1/2021. One checklist focused on health equity and SDOH and the second on cognitive biases. Both were incorporated into the section’s approved M&M templates utilized in the event review process. Each review was completed by a structured team of a GI fellow, faculty mentor and member of the section’s Quality and Safety team as per section standard. Presentations were tracked prospectively from 9/1/2021-5/30/2023 and content analyzed.
Results: Prior to the study period, there was no SDOH or cognitive bias content included in M&M presentations. A total of 12 presentations occurred during the study period. An average of 3.3 (range 0-8) SDOH-related factors and 3.8 (range 0-9) cognitive biases were found to contribute to reviewed events. Of the SDOH factors, 3 related to healthcare access, 4 were human factors, and 3 were psychosocial issues. The most common was healthcare provider interpretation of a clinical situation affecting an outcome, with patient substance use history being second most common. Of the cognitive biases, bandwagon effect caused by inheriting another’s line of thinking was most common. Two cases did not find any contributing SDOH and of these, one did not find any cognitive bias or deviation in care. All 12 presentations generated change ideas and 6 resulted in implemented changes. Only 3 action items focused on changes addressing SDOH and none of these resulted in implemented changes.
Discussion: Incorporating formalized checklists into M&M conferences can be an effective method to evaluate for impacts of SDOH and cognitive bias on adverse events and errors in a standardized and meaningful way. They also serve a second purpose to shift M&M towards a tool for culture transformation, just culture and story sharing to move health equity forward. More effort is needed to support routinely assessing the impact of bias and equity on adverse events in Gastroenterology to drive further change.
Disclosures:
Michelle Hughes: MotusGI – Consultant.
Carolyn Haight indicated no relevant financial relationships.
Aldo Peixoto: Ablative Solutions – Fees - Data Safety Monitoring Board. Bayer – Grant/Research Support. BD – Consultant. Boehringer Ingelheim – Grant/Research Support. Diamedica – Consultant. KBP Biosciences – Fees - Data Safety Monitoring Board. Lundbeck – Grant/Research Support. Reata – Grant/Research Support. Regeneron – Consultant.
Linda Fan indicated no relevant financial relationships.
Michelle L. Hughes, MD1, Carolyn Haight, MSN, RN, CPHQ2, Aldo Peixoto, MD1, Linda Fan, MD3. P1221 - Improving Identification of Social Determinants and Equity in Gastroenterology Adverse Events, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
