Sunday Poster Session
Category: Practice Management
P1241 - Finding Balance: Sharing the Workload Can Increase Turnover Efficiency and Cut Costs in the Endoscopy Unit
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Zoe Post, MD
Rush University Medical Center
Chicago, IL
Presenting Author(s)
Zoë Post, MD1, Prabakar Theivaraaj, MS1, Ajaypal Singh, MD2, Irving Waxman, MD1, Maham Lodhi, MD1, Neal Mehta, MD1
1Rush University Medical Center, Chicago, IL; 2Rush University Medical Group, Chicago, IL
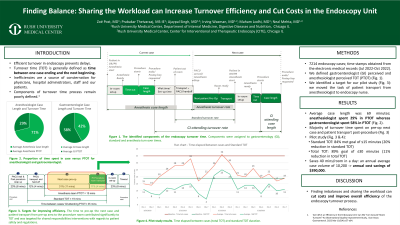
Introduction: To prevent delays in our tertiary endoscopy center, having an efficient turnover process is key. Turnover time (TOT) is generally defined as the amount of time between one case ending and another beginning. In figure 1, we have identified key components in TOT. Previously, our data has shown that the perceived TOT(PTOT) significantly varies between the different stakeholders(subgroups) that comprise the endoscopy team, including gastroenterologists, endoscopy nurses, anesthesiologists, and administrators. Initial data demonstrated an imbalance in workload between the anesthesia team and the endoscopy nurses, with the anesthesia team taking twice the amount of time than the nurses to finish their turnover tasks. This extended time is due to the anesthesia team being involved in all six components of the TOT pathway while the nursing team is only involved in three components. Thus, the anesthesia subgroup naturally creates a critical path with the longest lead time that dictates the TOT among all the subgroups. <span style="color: black; mso-themecolor: text1; mso-font-kerning: 0pt; mso-ligatures: none; mso-bidi-font-weight: bold;">In this study, we aimed to improve PTOT at a tertiary endoscopy center through optimal workload balance amongst the different subgroups.
Methods: Data for 7214 endoscopy cases with documented timestamps was collected to calculate the average TOT for various subgroups. To create the biggest impact amongst different TOT subgroups, we capitalized on one of the commonalities between them: patient transport (Figure 1 red box). To create balance, our intervention was to move the task of transporting the patient from the anesthesia nursing team to the endoscopy team (Figure 1), and we aimed to lower the standard TOT from 19 minutes to 15 minutes (20% reduction) and the time between cases from 35 to 31 minutes (11% reduction).
Results: In this pilot study, 19 individual turnovers were analyzed. For the standard TOT, 84% of the cases met the study goal of 15 minutes or less. For the total time between cases, 89% of the cases met the study goal of 30 minutes or less. On average, one procedure room in our center handles 10 cases per day. This intervention saved 40 mins/room in a day. With an annual average case volume of 10,200, this produces annual cost savings of about $390,000. It also expands the capacity of a procedure room by an additional 260 cases/year with a revenue potential of $180,000(if filled with procedures).
Discussion: Ultimately finding imbalances and sharing the workload can cut costs and improve the overall efficiency of the different subgroups in the turnover process.

Disclosures:
Zoë Post, MD1, Prabakar Theivaraaj, MS1, Ajaypal Singh, MD2, Irving Waxman, MD1, Maham Lodhi, MD1, Neal Mehta, MD1. P1241 - Finding Balance: Sharing the Workload Can Increase Turnover Efficiency and Cut Costs in the Endoscopy Unit, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Rush University Medical Center, Chicago, IL; 2Rush University Medical Group, Chicago, IL
Introduction: To prevent delays in our tertiary endoscopy center, having an efficient turnover process is key. Turnover time (TOT) is generally defined as the amount of time between one case ending and another beginning. In figure 1, we have identified key components in TOT. Previously, our data has shown that the perceived TOT(PTOT) significantly varies between the different stakeholders(subgroups) that comprise the endoscopy team, including gastroenterologists, endoscopy nurses, anesthesiologists, and administrators. Initial data demonstrated an imbalance in workload between the anesthesia team and the endoscopy nurses, with the anesthesia team taking twice the amount of time than the nurses to finish their turnover tasks. This extended time is due to the anesthesia team being involved in all six components of the TOT pathway while the nursing team is only involved in three components. Thus, the anesthesia subgroup naturally creates a critical path with the longest lead time that dictates the TOT among all the subgroups. <span style="color: black; mso-themecolor: text1; mso-font-kerning: 0pt; mso-ligatures: none; mso-bidi-font-weight: bold;">In this study, we aimed to improve PTOT at a tertiary endoscopy center through optimal workload balance amongst the different subgroups.
Methods: Data for 7214 endoscopy cases with documented timestamps was collected to calculate the average TOT for various subgroups. To create the biggest impact amongst different TOT subgroups, we capitalized on one of the commonalities between them: patient transport (Figure 1 red box). To create balance, our intervention was to move the task of transporting the patient from the anesthesia nursing team to the endoscopy team (Figure 1), and we aimed to lower the standard TOT from 19 minutes to 15 minutes (20% reduction) and the time between cases from 35 to 31 minutes (11% reduction).
Results: In this pilot study, 19 individual turnovers were analyzed. For the standard TOT, 84% of the cases met the study goal of 15 minutes or less. For the total time between cases, 89% of the cases met the study goal of 30 minutes or less. On average, one procedure room in our center handles 10 cases per day. This intervention saved 40 mins/room in a day. With an annual average case volume of 10,200, this produces annual cost savings of about $390,000. It also expands the capacity of a procedure room by an additional 260 cases/year with a revenue potential of $180,000(if filled with procedures).
Discussion: Ultimately finding imbalances and sharing the workload can cut costs and improve the overall efficiency of the different subgroups in the turnover process.

Figure: Figure 1. Top panel: perceived turnover times (PTOT) per subgroup and its components. Bottom panel: time between cases and standard TOT for individual cases observed during the pilot study.
Disclosures:
Zoë Post indicated no relevant financial relationships.
Prabakar Theivaraaj indicated no relevant financial relationships.
Ajaypal Singh indicated no relevant financial relationships.
Irving Waxman indicated no relevant financial relationships.
Maham Lodhi indicated no relevant financial relationships.
Neal Mehta indicated no relevant financial relationships.
Zoë Post, MD1, Prabakar Theivaraaj, MS1, Ajaypal Singh, MD2, Irving Waxman, MD1, Maham Lodhi, MD1, Neal Mehta, MD1. P1241 - Finding Balance: Sharing the Workload Can Increase Turnover Efficiency and Cut Costs in the Endoscopy Unit, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
