Sunday Poster Session
Category: Small Intestine
P1248 - Clinical Trial Failures in Inflammatory Bowel Disease: An Artificial Intelligence-Assisted Review
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio
- KN
Kingsley Njoku, MD, MS
Morehouse School of Medicine
Atlanta, GA
Presenting Author(s)
Kingsley Njoku, MD, MS1, Tesfaye Yadete, MD2, Joao Bettencourt-Silva, PhD3, Matthew T. Liu, 4, Vibha Anand, PhD5, Alberto Purpura, PhD3, Uri Kartoun, PhD6, Eileen Koski, MPhil7, Natasha Mulligan, MSc3, Brian Claggett, PhD8, Thaddeus Stappenbeck, MD, PhD9, Julia J.. Liu, MD1
1Morehouse School of Medicine, Atlanta, GA; 2Cleveland Clinic Foundation, Cleveland, OH; 3IBM Research, Dublin, Dublin, Ireland; 4Brown University, Providence, RI; 5IBD Research, Cambridge, MA; 6IBM Research, Cambridge, MA; 7IBM Research, Yorktown Heights, NY; 8Brigham and Women's Hospital, Boston, MA; 9Cleveland Clinic, Cleveland, OH
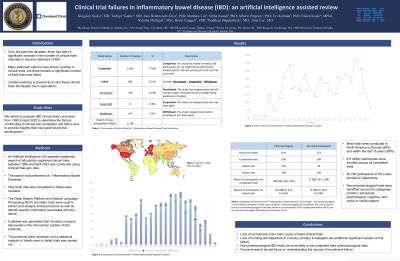
Introduction: Over the past few decades, there has been a significant increase in the number of clinical trials intended to improve treatment of inflammatory bowel disease (IBD). While some treatment options have shown promise in clinical trials, unfortunately, a significant number of trials have failed. There is much speculation as to why IBD clinical trials fail, but limited evidence has been presented. In this study, we aimed to evaluate IBD clinical trials conducted from 1999 to April 2023 to determine the factors contributing to clinical trial completion and failure and to provide insights that may guide future trial development.
Methods: An Artificial Intelligence (AI) assisted systematic search of publicly registered clinical trials between 1999 and April 2023 was conducted using ClinicalTrials.gov data. The search was performed on “Inflammatory Bowel Diseases” and only trials that were completed or failed were included. The Deep Search platform and Natural Language Processing (NLP) annotator tools were used to extract and analyze all trial protocols and identify specific information associated with trial failures. A dataset was generated that included concepts discovered in the intervention section of the trial protocols. These protocols were reviewed and a statistical analysis of trends seen in failed trials was carried out.
Results: Of the 1,734 IBD trials registered between 1999 and April 2023, 77.6% were completed (N=1,345) and 22.4% failed (N=389). 6.9 million participants were enrolled across all completed trials and only 30,782 (0.5%) were enrolled in failed trials. Completed pharmacological trials had a median of 100 participants enrolled (IQR: [40, 256]) while failed trials had a median of 16 participants (IQR:[0, 51]) with P< 0.001. Of 123 non-pharmacological trials, only 15% (N=19) failed. The median number of participants enrolled in completed trials was 71 (IQR: [41, 129]) and in failed trials was 3 (IQR:[0, 30]) with P< 0.001. The most common causes for failed non-pharmacological trials were failure to recruit patients (N=9), funding termination (N=3), and the principal investigator (PI) leaving the institution (N=2).
Discussion: Lack of recruitment is the main cause of failed clinical trials. Loss of funding and PI departure are additional significant causes of trial failures. Non-pharmacological IBD trials are more likely to be completed than pharmacological trials. Future research should focus on understanding causes of recruitment failures.
Disclosures:
Kingsley Njoku, MD, MS1, Tesfaye Yadete, MD2, Joao Bettencourt-Silva, PhD3, Matthew T. Liu, 4, Vibha Anand, PhD5, Alberto Purpura, PhD3, Uri Kartoun, PhD6, Eileen Koski, MPhil7, Natasha Mulligan, MSc3, Brian Claggett, PhD8, Thaddeus Stappenbeck, MD, PhD9, Julia J.. Liu, MD1. P1248 - Clinical Trial Failures in Inflammatory Bowel Disease: An Artificial Intelligence-Assisted Review, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Morehouse School of Medicine, Atlanta, GA; 2Cleveland Clinic Foundation, Cleveland, OH; 3IBM Research, Dublin, Dublin, Ireland; 4Brown University, Providence, RI; 5IBD Research, Cambridge, MA; 6IBM Research, Cambridge, MA; 7IBM Research, Yorktown Heights, NY; 8Brigham and Women's Hospital, Boston, MA; 9Cleveland Clinic, Cleveland, OH
Introduction: Over the past few decades, there has been a significant increase in the number of clinical trials intended to improve treatment of inflammatory bowel disease (IBD). While some treatment options have shown promise in clinical trials, unfortunately, a significant number of trials have failed. There is much speculation as to why IBD clinical trials fail, but limited evidence has been presented. In this study, we aimed to evaluate IBD clinical trials conducted from 1999 to April 2023 to determine the factors contributing to clinical trial completion and failure and to provide insights that may guide future trial development.
Methods: An Artificial Intelligence (AI) assisted systematic search of publicly registered clinical trials between 1999 and April 2023 was conducted using ClinicalTrials.gov data. The search was performed on “Inflammatory Bowel Diseases” and only trials that were completed or failed were included. The Deep Search platform and Natural Language Processing (NLP) annotator tools were used to extract and analyze all trial protocols and identify specific information associated with trial failures. A dataset was generated that included concepts discovered in the intervention section of the trial protocols. These protocols were reviewed and a statistical analysis of trends seen in failed trials was carried out.
Results: Of the 1,734 IBD trials registered between 1999 and April 2023, 77.6% were completed (N=1,345) and 22.4% failed (N=389). 6.9 million participants were enrolled across all completed trials and only 30,782 (0.5%) were enrolled in failed trials. Completed pharmacological trials had a median of 100 participants enrolled (IQR: [40, 256]) while failed trials had a median of 16 participants (IQR:[0, 51]) with P< 0.001. Of 123 non-pharmacological trials, only 15% (N=19) failed. The median number of participants enrolled in completed trials was 71 (IQR: [41, 129]) and in failed trials was 3 (IQR:[0, 30]) with P< 0.001. The most common causes for failed non-pharmacological trials were failure to recruit patients (N=9), funding termination (N=3), and the principal investigator (PI) leaving the institution (N=2).
Discussion: Lack of recruitment is the main cause of failed clinical trials. Loss of funding and PI departure are additional significant causes of trial failures. Non-pharmacological IBD trials are more likely to be completed than pharmacological trials. Future research should focus on understanding causes of recruitment failures.
Disclosures:
Kingsley Njoku indicated no relevant financial relationships.
Tesfaye Yadete indicated no relevant financial relationships.
Joao Bettencourt-Silva: IBM Research – Employee.
Matthew Liu indicated no relevant financial relationships.
Vibha Anand indicated no relevant financial relationships.
Alberto Purpura indicated no relevant financial relationships.
Uri Kartoun indicated no relevant financial relationships.
Eileen Koski indicated no relevant financial relationships.
Natasha Mulligan indicated no relevant financial relationships.
Brian Claggett: Alnylam – Consultant. Cardurion – Consultant. Corvia – Consultant. Cytokinetics – Consultant. Intellia – Consultant. Novartis – Consultant. Rocket – Consultant.
Thaddeus Stappenbeck indicated no relevant financial relationships.
Julia Liu indicated no relevant financial relationships.
Kingsley Njoku, MD, MS1, Tesfaye Yadete, MD2, Joao Bettencourt-Silva, PhD3, Matthew T. Liu, 4, Vibha Anand, PhD5, Alberto Purpura, PhD3, Uri Kartoun, PhD6, Eileen Koski, MPhil7, Natasha Mulligan, MSc3, Brian Claggett, PhD8, Thaddeus Stappenbeck, MD, PhD9, Julia J.. Liu, MD1. P1248 - Clinical Trial Failures in Inflammatory Bowel Disease: An Artificial Intelligence-Assisted Review, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
