Sunday Poster Session
Category: Small Intestine
P1269 - A Rare Case of Primary Duodenal Adenocarcinoma
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Aizaz Khan, MD
University of Massachusetts Chan Medical School-Baystate
Springfield, Massachusetts
Presenting Author(s)
Aizaz Khan, MD1, Bushra Zia, MD2, Rony Ghaoui, MD1
1University of Massachusetts Chan Medical School-Baystate, Springfield, MA; 2Holyoke Medical Center, Springfield, MA
Introduction: Small bowel malignancies are exceedingly rare with incidence of primary small bowel adenocarcinoma (SBA) in the US estimated to be 3.9 cases per million persons. Typical presenting features are nonspecific and range from abdominal pain and nausea/vomiting to GI bleeds and intestinal obstruction. We present a unique case of SBA which presented as biliary obstruction with jaundice.
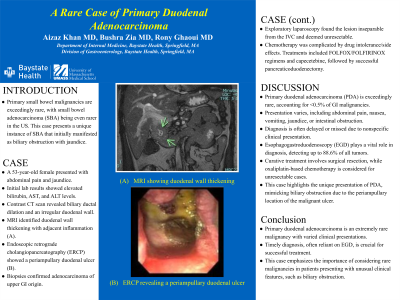
Case Description/Methods: A 53-year-old female presented to our facility with abdominal pain and was noted to have jaundice on exam. Initial blood work was notable for total bilirubin 2.8mg/dl along with aspartate aminotransferase (AST) of 350 units/L and alanine aminotransferase (ALT) of 678 units/L . A contrasted computed tomography (CT) scan of the abdomen and pelvis showed intra and extrahepatic biliary ductal dilation and common bile duct diameter of 10mm. Intrahepatic ducts were noted to be irregular and tortuous. Due to the irregularities noted on CT, magnetic resonance imaging (MRI) was performed revealing wall thickening of the second portion of the duodenum with adjacent inflammatory changes. The patient underwent endoscopic retrograde cholangiopancreatography (ERCP) which showed a periampullary duodenal ulcer. Biopsies were obtained and cholangiogram was attempted but failed. Pathology of the duodenal biopsy was diagnostic for adenocarcinoma of upper GI origin. She subsequently underwent exploratory laparoscopy however her duodenal lesion was found to be inseparable from the IVC and therefore deemed unresectable initially. She eventually completed therapy with FOLFOX, FOLFIRINOX, and capecetebine. Post-treatment completion she was able to undergo successful pancreaticoduodonectomy.
Discussion: Primary duodenal adenocarcinoma (PDA) is a very rare tumor accounting for less than 0.5% of GI tract malignancies. The location of the tumor determines the presenting features such as abdominal pain, nausea, vomiting, jaundice, or intestinal obstruction. Due to the varying and nonspecific clinical presentation of PDA, diagnosis is often delayed or missed. CT imaging has an overall accuracy of 47% for diagnosis with esophagogastroduodenoscopy (EGD) holding a more key role in diagnosis detecting up to 88.6% of all tumors. Curative treatment is through surgical resection. Oxaliplatin chemotherapeutic regiments have also been described for patients with unresectable tumors. Our case highlights the unique presentation of PDA mimicking biliary obstruction due to the periampullary location of the malignant ulcer.

Disclosures:
Aizaz Khan, MD1, Bushra Zia, MD2, Rony Ghaoui, MD1. P1269 - A Rare Case of Primary Duodenal Adenocarcinoma, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Massachusetts Chan Medical School-Baystate, Springfield, MA; 2Holyoke Medical Center, Springfield, MA
Introduction: Small bowel malignancies are exceedingly rare with incidence of primary small bowel adenocarcinoma (SBA) in the US estimated to be 3.9 cases per million persons. Typical presenting features are nonspecific and range from abdominal pain and nausea/vomiting to GI bleeds and intestinal obstruction. We present a unique case of SBA which presented as biliary obstruction with jaundice.
Case Description/Methods: A 53-year-old female presented to our facility with abdominal pain and was noted to have jaundice on exam. Initial blood work was notable for total bilirubin 2.8mg/dl along with aspartate aminotransferase (AST) of 350 units/L and alanine aminotransferase (ALT) of 678 units/L . A contrasted computed tomography (CT) scan of the abdomen and pelvis showed intra and extrahepatic biliary ductal dilation and common bile duct diameter of 10mm. Intrahepatic ducts were noted to be irregular and tortuous. Due to the irregularities noted on CT, magnetic resonance imaging (MRI) was performed revealing wall thickening of the second portion of the duodenum with adjacent inflammatory changes. The patient underwent endoscopic retrograde cholangiopancreatography (ERCP) which showed a periampullary duodenal ulcer. Biopsies were obtained and cholangiogram was attempted but failed. Pathology of the duodenal biopsy was diagnostic for adenocarcinoma of upper GI origin. She subsequently underwent exploratory laparoscopy however her duodenal lesion was found to be inseparable from the IVC and therefore deemed unresectable initially. She eventually completed therapy with FOLFOX, FOLFIRINOX, and capecetebine. Post-treatment completion she was able to undergo successful pancreaticoduodonectomy.
Discussion: Primary duodenal adenocarcinoma (PDA) is a very rare tumor accounting for less than 0.5% of GI tract malignancies. The location of the tumor determines the presenting features such as abdominal pain, nausea, vomiting, jaundice, or intestinal obstruction. Due to the varying and nonspecific clinical presentation of PDA, diagnosis is often delayed or missed. CT imaging has an overall accuracy of 47% for diagnosis with esophagogastroduodenoscopy (EGD) holding a more key role in diagnosis detecting up to 88.6% of all tumors. Curative treatment is through surgical resection. Oxaliplatin chemotherapeutic regiments have also been described for patients with unresectable tumors. Our case highlights the unique presentation of PDA mimicking biliary obstruction due to the periampullary location of the malignant ulcer.

Figure: Magnetic resonance imaging of the abdomen showing irregular wall thickening of the second part of the duodenum abutting the IVC
Disclosures:
Aizaz Khan indicated no relevant financial relationships.
Bushra Zia indicated no relevant financial relationships.
Rony Ghaoui indicated no relevant financial relationships.
Aizaz Khan, MD1, Bushra Zia, MD2, Rony Ghaoui, MD1. P1269 - A Rare Case of Primary Duodenal Adenocarcinoma, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
