Sunday Poster Session
Category: Small Intestine
P1274 - A Rare Case of Non-Celiac Adult-Onset Autoimmune Enteropathy With Villous Atrophy
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio
- ZY
Zarqa Yasin, MD
Henry Ford Health
Jackson, MI
Presenting Author(s)
Zarqa Yasin, MD1, Parneet Hari, MD2, Hassan Zreik, MD2, Parth M. Patel, MD3, Bipneet Singh, MD1, Nadeem Ullah, MD4
1Henry Ford Health, Jackson, MI; 2Henry Ford Health System, Jackson, MI; 3Henry Ford Health System, Boston, MA; 4Henry Ford Jackson Hospital, Jackson, MI
Introduction: Autoimmune enteropathy (AIE) is a rare and often underdiagnosed condition characterized by persistent diarrhea, severe malabsorption, small intestinal villous atrophy, and symptoms mimicking refractory celiac disease. This case report focuses on adult-onset AIE and highlights the challenges in diagnosing and managing this condition due to its varied clinical and pathological presentations.
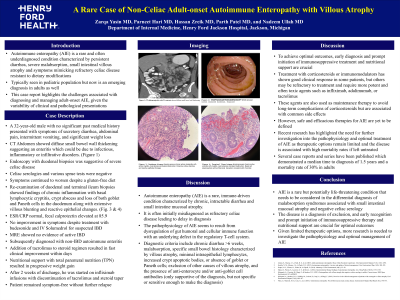
Case Description/Methods: A 32-year-old male presented with worsening secretory diarrhea, abdominal pain, intermittent vomiting, and significant weight loss. Imaging revealed diffuse small bowel wall thickening, suggesting enteritis. Initial duodenal biopsies indicated severe celiac disease, but celiac serologies and sprue tests were negative. Despite adhering to a gluten-free diet, symptoms persisted. Subsequent reexamination of the biopsies revealed chronic inflammation with basal lymphocytic cryptitis, crypt abscesses, loss of goblet and Paneth cells in the duodenum, extensive villous blunting, and reactive epithelial changes were observed. Inflammatory markers were within normal range, while fecal calprotectin was elevated. Suspecting inflammatory bowel disease (IBD), treatment with corticosteroids yielded no improvement. Magnetic resonance enterography ruled out active IBD. Ultimately, the patient was diagnosed with autoimmune enteropathy through a process of exclusion. Adding tacrolimus to the steroid regimen led to rapid clinical improvement and nutritional support through TPN aided in weight gain. Following discharge, patient received infliximab infusions and remained symptom-free.
Discussion: Adult autoimmune enteropathy (AIE) is a rare condition with limited data, mainly from case reports and small case series. The diagnostic criteria for AIE are still uncertain, and autoantibodies may not always be detectable. Dysfunction of the intestinal immune system is believed to be the underlying cause. Histological analysis has identified different subtypes of AIE, including active chronic enteritis and celiac disease-like patterns, along with colonic inflammation.
Managing AIE can be challenging, as response rates to corticosteroids and immunomodulators vary. However, the optimal treatment strategies for AIE remain undefined, emphasizing the need for further research. If left untreated, AIE can result in high mortality rates, underscoring the importance of early diagnosis and intervention. Reporting and studying cases are crucial for improving our understanding and enhancing patient outcomes.

Disclosures:
Zarqa Yasin, MD1, Parneet Hari, MD2, Hassan Zreik, MD2, Parth M. Patel, MD3, Bipneet Singh, MD1, Nadeem Ullah, MD4. P1274 - A Rare Case of Non-Celiac Adult-Onset Autoimmune Enteropathy With Villous Atrophy, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Henry Ford Health, Jackson, MI; 2Henry Ford Health System, Jackson, MI; 3Henry Ford Health System, Boston, MA; 4Henry Ford Jackson Hospital, Jackson, MI
Introduction: Autoimmune enteropathy (AIE) is a rare and often underdiagnosed condition characterized by persistent diarrhea, severe malabsorption, small intestinal villous atrophy, and symptoms mimicking refractory celiac disease. This case report focuses on adult-onset AIE and highlights the challenges in diagnosing and managing this condition due to its varied clinical and pathological presentations.
Case Description/Methods: A 32-year-old male presented with worsening secretory diarrhea, abdominal pain, intermittent vomiting, and significant weight loss. Imaging revealed diffuse small bowel wall thickening, suggesting enteritis. Initial duodenal biopsies indicated severe celiac disease, but celiac serologies and sprue tests were negative. Despite adhering to a gluten-free diet, symptoms persisted. Subsequent reexamination of the biopsies revealed chronic inflammation with basal lymphocytic cryptitis, crypt abscesses, loss of goblet and Paneth cells in the duodenum, extensive villous blunting, and reactive epithelial changes were observed. Inflammatory markers were within normal range, while fecal calprotectin was elevated. Suspecting inflammatory bowel disease (IBD), treatment with corticosteroids yielded no improvement. Magnetic resonance enterography ruled out active IBD. Ultimately, the patient was diagnosed with autoimmune enteropathy through a process of exclusion. Adding tacrolimus to the steroid regimen led to rapid clinical improvement and nutritional support through TPN aided in weight gain. Following discharge, patient received infliximab infusions and remained symptom-free.
Discussion: Adult autoimmune enteropathy (AIE) is a rare condition with limited data, mainly from case reports and small case series. The diagnostic criteria for AIE are still uncertain, and autoantibodies may not always be detectable. Dysfunction of the intestinal immune system is believed to be the underlying cause. Histological analysis has identified different subtypes of AIE, including active chronic enteritis and celiac disease-like patterns, along with colonic inflammation.
Managing AIE can be challenging, as response rates to corticosteroids and immunomodulators vary. However, the optimal treatment strategies for AIE remain undefined, emphasizing the need for further research. If left untreated, AIE can result in high mortality rates, underscoring the importance of early diagnosis and intervention. Reporting and studying cases are crucial for improving our understanding and enhancing patient outcomes.

Figure: Figure 1: CT abdomen/pelvis with IV contrast showed diffuse small bowel wall thickening. Figure 2: EGD showed normal duodenum which was biopsied. Figure 3: Duodenum biopsy showing severe chronic active duodenitis with active cryptitis, crypt abscess and gland destruction as well as extensive villous blunting and reactive epithelial changes.
Disclosures:
Zarqa Yasin indicated no relevant financial relationships.
Parneet Hari indicated no relevant financial relationships.
Hassan Zreik indicated no relevant financial relationships.
Parth Patel indicated no relevant financial relationships.
Bipneet Singh indicated no relevant financial relationships.
Nadeem Ullah indicated no relevant financial relationships.
Zarqa Yasin, MD1, Parneet Hari, MD2, Hassan Zreik, MD2, Parth M. Patel, MD3, Bipneet Singh, MD1, Nadeem Ullah, MD4. P1274 - A Rare Case of Non-Celiac Adult-Onset Autoimmune Enteropathy With Villous Atrophy, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
