Sunday Poster Session
Category: Small Intestine
P1275 - Dermatomyositis-Associated Gastrointestinal Cancer Presenting as Pulmonary Hypertension
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Allison Derise, MD
Louisiana State University Health Sciences Center
New Orleans, LA
Presenting Author(s)
Allison Derise, MD1, Amy Wolfe, MD2, Matthew Lammi, MD, MSCR2
1Louisiana State University Health Sciences Center, New Orleans, LA; 2LSU Health Sciences Center, New Orleans, LA
Introduction: Pulmonary hypertension (PH) caused by tumor emboli is classified by two subgroups: pulmonary tumor microembolism (PTE) and pulmonary tumor thrombotic microangiopathy (PTTM) and is most often found postmortem. PTE is described as pulmonary microvascular occlusion by tumor thrombi. PTTM is caused by pulmonary vasculature remodeling caused by tumor emboli. Both of these can cause PH, and it is usually rapid, progressive, and fatal. Of the case reports of these diseases, most have been linked with gastric cancer. Gastric and colorectal cancers are malignancies also known to be strongly associated with dermatomyositis, and there are certain antibodies related to increased incidence of malignancies. This case report discusses a patient with presumed dermatomyositis-associated gastrointestinal cancer presenting as severe PH and the supporting evidence of this diagnosis.
Case Description/Methods: This patient was a 64-year-old male who was transferred to our hospital for management of acute hypoxic respiratory failure and severe PH. He initially presented with severe shortness of breath, dyspnea on exertion, easy fatiguability, nausea, and a 70-lb weight loss over the prior 3 months. He also reported a rash on his knuckles and elbows for the last 6 months. His physical exam was notable for bilateral lower extremity edema, TR murmur, and purple papules on bilateral MCP joints.
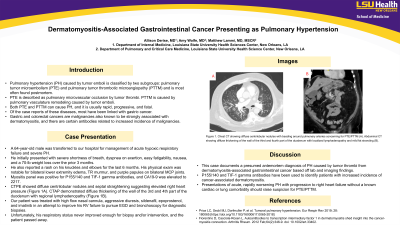
Myositis panel was positive for P155/140 and TIF-1 gamma antibodies, and CA19-9 was elevated to 2217. CTPE showed diffuse centrilobular nodules and septal straightening suggesting elevated right heart pressure (Figure 1A). CTAP demonstrated diffuse thickening of the wall of the 3rd and 4th part of the duodenum with regional lymphadenopathy (Figure 1B).
Our patient was treated with high flow nasal cannula, aggressive diuresis, sildenafil, epoprostenol, and imatinib in an attempt to improve his RV failure to pursue EGD and bronchoscopy for diagnostic biopsies. Unfortunately, his respiratory status never improved enough, and the patient passed away.
Discussion: This case documents a presumed antemortem diagnosis of PH caused by tumor thrombi from dermatomyositis-associated gastrointestinal cancer based off of lab and imaging findings. P155/140 and TIF-1 gamma antibodies have been used to identify patients with increased incidence of cancer-associated dermatomyositis. Presentations of acute, rapidly worsening PH with progression to right heart failure without a known cardiac or lung comorbidity should raise suspicion for PTE/PTTM.

Disclosures:
Allison Derise, MD1, Amy Wolfe, MD2, Matthew Lammi, MD, MSCR2. P1275 - Dermatomyositis-Associated Gastrointestinal Cancer Presenting as Pulmonary Hypertension, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Louisiana State University Health Sciences Center, New Orleans, LA; 2LSU Health Sciences Center, New Orleans, LA
Introduction: Pulmonary hypertension (PH) caused by tumor emboli is classified by two subgroups: pulmonary tumor microembolism (PTE) and pulmonary tumor thrombotic microangiopathy (PTTM) and is most often found postmortem. PTE is described as pulmonary microvascular occlusion by tumor thrombi. PTTM is caused by pulmonary vasculature remodeling caused by tumor emboli. Both of these can cause PH, and it is usually rapid, progressive, and fatal. Of the case reports of these diseases, most have been linked with gastric cancer. Gastric and colorectal cancers are malignancies also known to be strongly associated with dermatomyositis, and there are certain antibodies related to increased incidence of malignancies. This case report discusses a patient with presumed dermatomyositis-associated gastrointestinal cancer presenting as severe PH and the supporting evidence of this diagnosis.
Case Description/Methods: This patient was a 64-year-old male who was transferred to our hospital for management of acute hypoxic respiratory failure and severe PH. He initially presented with severe shortness of breath, dyspnea on exertion, easy fatiguability, nausea, and a 70-lb weight loss over the prior 3 months. He also reported a rash on his knuckles and elbows for the last 6 months. His physical exam was notable for bilateral lower extremity edema, TR murmur, and purple papules on bilateral MCP joints.
Myositis panel was positive for P155/140 and TIF-1 gamma antibodies, and CA19-9 was elevated to 2217. CTPE showed diffuse centrilobular nodules and septal straightening suggesting elevated right heart pressure (Figure 1A). CTAP demonstrated diffuse thickening of the wall of the 3rd and 4th part of the duodenum with regional lymphadenopathy (Figure 1B).
Our patient was treated with high flow nasal cannula, aggressive diuresis, sildenafil, epoprostenol, and imatinib in an attempt to improve his RV failure to pursue EGD and bronchoscopy for diagnostic biopsies. Unfortunately, his respiratory status never improved enough, and the patient passed away.
Discussion: This case documents a presumed antemortem diagnosis of PH caused by tumor thrombi from dermatomyositis-associated gastrointestinal cancer based off of lab and imaging findings. P155/140 and TIF-1 gamma antibodies have been used to identify patients with increased incidence of cancer-associated dermatomyositis. Presentations of acute, rapidly worsening PH with progression to right heart failure without a known cardiac or lung comorbidity should raise suspicion for PTE/PTTM.

Figure: Figure 1. Chest CT showing diffuse centrilobular nodules with beading around pulmonary arteries concerning for PTE/PTTM (A). Abdominal CT showing diffuse thickening of the wall of the third and fourth part of the duodenum with localized lymphadenopathy and mild fat stranding (B).
Disclosures:
Allison Derise indicated no relevant financial relationships.
Amy Wolfe indicated no relevant financial relationships.
Matthew Lammi indicated no relevant financial relationships.
Allison Derise, MD1, Amy Wolfe, MD2, Matthew Lammi, MD, MSCR2. P1275 - Dermatomyositis-Associated Gastrointestinal Cancer Presenting as Pulmonary Hypertension, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
