Sunday Poster Session
Category: Small Intestine
P1278 - Ileocecal Stricture as a Manifestation of Disseminated Histoplasmosis in an Immunosuppressed Patient: A Case Report
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Christine Catinis, MD, MS
University of Texas Health Science Center at Houston
Houston, TX
Presenting Author(s)
Christine Catinis, MD, MS1, Christopher Fernandes, BSc2, Maya Sarihan, MD1, Abdullah Aleem, MD3, Parvir Aujla, MD4, Precious Anyanwu, PharmD, PhD5, Timothy E.. Ritter, MD6
1University of Texas Health Science Center at Houston, Houston, TX; 2Anne Burnett Marion School of Medicine at TCU, Fort Worth, TX; 3University of Texas Health Science Center, Houston, AZ; 4University of Texas Health Science Center, Houston, TX; 5Healix, LLC, Houston, TX; 6GI Alliance, Southlake, TX
Introduction: Histoplasmosis is an endemic fungal disease caused by the dimorphic fungus, Histoplasma capsulatum. In immunocompromised individuals, it can spread from the lungs throughout the body via macrophages, leading to disseminated disease which can affect multiple organ systems. Here, we describe a case of intestinal stricture as a manifestation of disseminated histoplasmosis in an immunosuppressed patient with Crohn’s disease (CD).
Case Description/Methods: Our patient is a 74 y/o male with a history of severe perianal fistulizing CD who has been in remission on infliximab and mercaptopurine for the past decade. He initially presented with a 5-month history of fevers, fatigue, and marked weight loss, though multiple physician evaluations failed to reveal a cause for his presentation. Ultimately, he developed a profound pancytopenia requiring blood transfusions and a bone marrow biopsy, and a urine antigen test confirmed a diagnosis of histoplasmosis. Infliximab was discontinued, and he was first treated with intravenous (IV) and subsequently oral itraconazole with improvement of his symptoms and resolution of his pancytopenia. A few months later he developed recurrent abdominal pain, vomiting, and weight loss. He had multiple ED visits for presumed small bowel obstructions (SBOs) that quickly resolved with conservative therapy. After several episodes, he developed a SBO that failed to resolve and underwent surgical evaluation which showed two distinct ileal strictures. The pathology for the distal ileal stricture was typical for active ileal CD. The pathology of the proximal stricture, however, showed multiple tiny yeast-like microorganisms associated with granulomata, with fungal staining revealed gastrointestinal histoplasmosis. The patient ultimately was maintained on oral itraconazole, and started on Risankizumab for his CD.
Discussion: There are very few published reports of ileal stenosis secondary to histoplasmosis, and it has rarely been reported to cause SBO. Given our patient’s history of fistulizing inflammatory bowel disease (IBD), his presentation of SBO secondary to an ileal stricture could have been attributed to his Crohn’s disease. Our case illustrates why diagnosis of GI histoplasmosis can often be delayed in IBD patients given the significant overlap in clinical manifestations and pathologic findings. Early diagnosis with endoscopic biopsy and prompt treatment is paramount in preventing severe complications such as bowel perforation, hemorrhage, and progressive fungal infection.

Disclosures:
Christine Catinis, MD, MS1, Christopher Fernandes, BSc2, Maya Sarihan, MD1, Abdullah Aleem, MD3, Parvir Aujla, MD4, Precious Anyanwu, PharmD, PhD5, Timothy E.. Ritter, MD6. P1278 - Ileocecal Stricture as a Manifestation of Disseminated Histoplasmosis in an Immunosuppressed Patient: A Case Report, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Texas Health Science Center at Houston, Houston, TX; 2Anne Burnett Marion School of Medicine at TCU, Fort Worth, TX; 3University of Texas Health Science Center, Houston, AZ; 4University of Texas Health Science Center, Houston, TX; 5Healix, LLC, Houston, TX; 6GI Alliance, Southlake, TX
Introduction: Histoplasmosis is an endemic fungal disease caused by the dimorphic fungus, Histoplasma capsulatum. In immunocompromised individuals, it can spread from the lungs throughout the body via macrophages, leading to disseminated disease which can affect multiple organ systems. Here, we describe a case of intestinal stricture as a manifestation of disseminated histoplasmosis in an immunosuppressed patient with Crohn’s disease (CD).
Case Description/Methods: Our patient is a 74 y/o male with a history of severe perianal fistulizing CD who has been in remission on infliximab and mercaptopurine for the past decade. He initially presented with a 5-month history of fevers, fatigue, and marked weight loss, though multiple physician evaluations failed to reveal a cause for his presentation. Ultimately, he developed a profound pancytopenia requiring blood transfusions and a bone marrow biopsy, and a urine antigen test confirmed a diagnosis of histoplasmosis. Infliximab was discontinued, and he was first treated with intravenous (IV) and subsequently oral itraconazole with improvement of his symptoms and resolution of his pancytopenia. A few months later he developed recurrent abdominal pain, vomiting, and weight loss. He had multiple ED visits for presumed small bowel obstructions (SBOs) that quickly resolved with conservative therapy. After several episodes, he developed a SBO that failed to resolve and underwent surgical evaluation which showed two distinct ileal strictures. The pathology for the distal ileal stricture was typical for active ileal CD. The pathology of the proximal stricture, however, showed multiple tiny yeast-like microorganisms associated with granulomata, with fungal staining revealed gastrointestinal histoplasmosis. The patient ultimately was maintained on oral itraconazole, and started on Risankizumab for his CD.
Discussion: There are very few published reports of ileal stenosis secondary to histoplasmosis, and it has rarely been reported to cause SBO. Given our patient’s history of fistulizing inflammatory bowel disease (IBD), his presentation of SBO secondary to an ileal stricture could have been attributed to his Crohn’s disease. Our case illustrates why diagnosis of GI histoplasmosis can often be delayed in IBD patients given the significant overlap in clinical manifestations and pathologic findings. Early diagnosis with endoscopic biopsy and prompt treatment is paramount in preventing severe complications such as bowel perforation, hemorrhage, and progressive fungal infection.

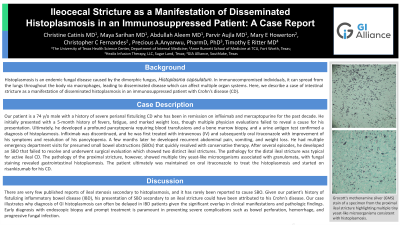
Figure: Grocott's methenamine silver (GMS) stain of a specimen from the proximal ileal stricture highlighting multiple tiny yeast-like microorganisms consistent with histoplasmosis.
Disclosures:
Christine Catinis indicated no relevant financial relationships.
Christopher Fernandes indicated no relevant financial relationships.
Maya Sarihan indicated no relevant financial relationships.
Abdullah Aleem indicated no relevant financial relationships.
Parvir Aujla indicated no relevant financial relationships.
Precious Anyanwu indicated no relevant financial relationships.
Timothy Ritter: Abbvie – Advisory Committee/Board Member, Speakers Bureau. ArdelyxArena – Advisory Committee/Board Member. Boehringer Ingelheim – Advisory Committee/Board Member. Bristol-Myers Squibb – Advisory Committee/Board Member, Speakers Bureau. Celgene – Advisory Committee/Board Member. Ferring – Advisory Committee/Board Member. Genentech/Roche Gilead – Advisory Committee/Board Member. Intercept – Advisory Committee/Board Member. Iterative Scopes – Advisory Committee/Board Member, Stock-publicly held company(excluding mutual/index funds). Janssen – Advisory Committee/Board Member, Speakers Bureau. Lilly – Advisory Committee/Board Member. Pfizer inc – Advisory Committee/Board Member, Speakers Bureau. Prometheus Biosciences – Advisory Committee/Board Member. Sanofi – Advisory Committee/Board Member. Takeda – Advisory Committee/Board Member, Speakers Bureau.
Christine Catinis, MD, MS1, Christopher Fernandes, BSc2, Maya Sarihan, MD1, Abdullah Aleem, MD3, Parvir Aujla, MD4, Precious Anyanwu, PharmD, PhD5, Timothy E.. Ritter, MD6. P1278 - Ileocecal Stricture as a Manifestation of Disseminated Histoplasmosis in an Immunosuppressed Patient: A Case Report, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
