Sunday Poster Session
Category: Small Intestine
P1280 - Clostridioides difficile Enteritis a Rare but Deadly Diagnosis
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Nehal Patel, MD
Rosalind Franklin University of Medicine and Science
Chicago, IL
Presenting Author(s)
Nehal Patel, MD1, Alexander Magasic, MD2, Swetha Paduri, MD1, Peter Morawiecki, MD3, Paul Roach, MD4
1Rosalind Franklin University of Medicine and Science, Chicago, IL; 2Ross University, Chicago, IL; 3Captain James A. Lovell Federal Health Care Center, North Chicago, IL; 4Captain James A. Lovell Federal Health Care Center, Chicago, IL
Introduction: Clostridium difficile infection (CDI) is one of the most prevalent nosocomial infections and accounts for more than 80% of morbidity in the geriatric population. CDIs can happen at any age, especially in those who are colonized and undergo disruption of the gut flora. CDI has wide and varied manifestations from asymptomatic to fulminant colitis. This is a case of CDI with exclusive extracolonic involvement in the absence of gastrointestinal surgery.
Case Description/Methods: A 30-year-old female with a history of uterine fibroids presented with a 2-day history of abdominal pain and large-volume diarrhea and she had undergone a myomectomy 5 days prior to presentation. CT imaging showed findings consistent with a high-grade small bowel obstruction. An urgent exploratory laparotomy revealed dilated small bowel with remnants of fibrous bands in the ileum which was lysed upon evisceration. The patient was treated with empiric antibiotics and fluid resuscitation. She had persistent hypotension which was considered a sequela of increased intra-abdominal pressure. She subsequently returned to the OR for a repeat exploratory laparotomy to rule out bowel ischemia. Operative findings included an 80 cm segment of ischemic distal jejunum and proximal ileum with patchy areas of necrosis and serosal tears. Now, stool studies returned positive for CDI, and treatment with oral vancomycin was initiated. Her third laparotomy with a planned abdominal closure demonstrated further edema of the distal small bowel with areas of necrosis, resulting in further resection. Ultimately, only 75 cm of distal small bowel remained. Histopathology revealed mucosal necrosis with abundant inflammation and vascular thrombi. These findings were consistent with C. difficile enteritis.
Discussion: CDI usually manifests in the colon. Colonization of the intestinal tract occurs via the fecal-oral route. In this case, the patient was prophylactically treated with cefoxitin prior to surgery. It is plausible that she was previously colonized and the introduction to antibiotics led to fulminant CDI. Small bowel involvement with CDI enteritis is extremely rare, even more so, in the absence of colonic surgery. To date, there are less than 100 cases of C. difficile enteritis, with nearly no reported cases in the absence of colectomies. Cases of isolated C. difficile enteritis require intense monitoring with a multidisciplinary approach as they carry a significantly higher morbidity and mortality rates compared to colonic CDI manifestations.

Disclosures:
Nehal Patel, MD1, Alexander Magasic, MD2, Swetha Paduri, MD1, Peter Morawiecki, MD3, Paul Roach, MD4. P1280 - Clostridioides difficile Enteritis a Rare but Deadly Diagnosis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Rosalind Franklin University of Medicine and Science, Chicago, IL; 2Ross University, Chicago, IL; 3Captain James A. Lovell Federal Health Care Center, North Chicago, IL; 4Captain James A. Lovell Federal Health Care Center, Chicago, IL
Introduction: Clostridium difficile infection (CDI) is one of the most prevalent nosocomial infections and accounts for more than 80% of morbidity in the geriatric population. CDIs can happen at any age, especially in those who are colonized and undergo disruption of the gut flora. CDI has wide and varied manifestations from asymptomatic to fulminant colitis. This is a case of CDI with exclusive extracolonic involvement in the absence of gastrointestinal surgery.
Case Description/Methods: A 30-year-old female with a history of uterine fibroids presented with a 2-day history of abdominal pain and large-volume diarrhea and she had undergone a myomectomy 5 days prior to presentation. CT imaging showed findings consistent with a high-grade small bowel obstruction. An urgent exploratory laparotomy revealed dilated small bowel with remnants of fibrous bands in the ileum which was lysed upon evisceration. The patient was treated with empiric antibiotics and fluid resuscitation. She had persistent hypotension which was considered a sequela of increased intra-abdominal pressure. She subsequently returned to the OR for a repeat exploratory laparotomy to rule out bowel ischemia. Operative findings included an 80 cm segment of ischemic distal jejunum and proximal ileum with patchy areas of necrosis and serosal tears. Now, stool studies returned positive for CDI, and treatment with oral vancomycin was initiated. Her third laparotomy with a planned abdominal closure demonstrated further edema of the distal small bowel with areas of necrosis, resulting in further resection. Ultimately, only 75 cm of distal small bowel remained. Histopathology revealed mucosal necrosis with abundant inflammation and vascular thrombi. These findings were consistent with C. difficile enteritis.
Discussion: CDI usually manifests in the colon. Colonization of the intestinal tract occurs via the fecal-oral route. In this case, the patient was prophylactically treated with cefoxitin prior to surgery. It is plausible that she was previously colonized and the introduction to antibiotics led to fulminant CDI. Small bowel involvement with CDI enteritis is extremely rare, even more so, in the absence of colonic surgery. To date, there are less than 100 cases of C. difficile enteritis, with nearly no reported cases in the absence of colectomies. Cases of isolated C. difficile enteritis require intense monitoring with a multidisciplinary approach as they carry a significantly higher morbidity and mortality rates compared to colonic CDI manifestations.

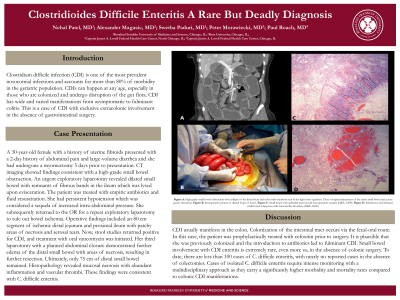
Figure: Figure A: High-grade small bowel obstruction with collapse of the distal ileum and colon with transition seen in the right lower quadrant. There is hyperenhancement of the entire small bowel and severe gastric distention.
Figure B: Intraoperative picture of dilated loops of bowel
Figure C: Small bowel with epithelial necrosis and mucopurulent exudate (H&E, X400)
Figure D: Edematous and inflamed small bowel submucosa with intravascular thrombus (H&E, X400)
Figure B: Intraoperative picture of dilated loops of bowel
Figure C: Small bowel with epithelial necrosis and mucopurulent exudate (H&E, X400)
Figure D: Edematous and inflamed small bowel submucosa with intravascular thrombus (H&E, X400)
Disclosures:
Nehal Patel indicated no relevant financial relationships.
Alexander Magasic indicated no relevant financial relationships.
Swetha Paduri indicated no relevant financial relationships.
Peter Morawiecki indicated no relevant financial relationships.
Paul Roach indicated no relevant financial relationships.
Nehal Patel, MD1, Alexander Magasic, MD2, Swetha Paduri, MD1, Peter Morawiecki, MD3, Paul Roach, MD4. P1280 - Clostridioides difficile Enteritis a Rare but Deadly Diagnosis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
