Sunday Poster Session
Category: Small Intestine
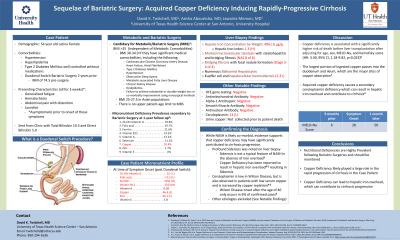
P1307 - Sequelae of Bariatric Surgery: Acquired Copper Deficiency Inducing Rapidly-Progressive Cirrhosis
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio
David Twitchell, MD
UT Health San Antonio
San Antonio, TX
Presenting Author(s)
David Twitchell, MD1, Aesha Aboueisha, MD2, Jawairia Memon, MD3
1UT Health San Antonio, San Antonio, TX; 2University of Texas Health Science Center at San Antonio, San Antonio, TX; 3University of Texas Health Science Center San Antonio, San Antonio, TX
Introduction: Weight-loss, or bariatric, surgery is recommended for patients with BMI >35 or >30 if they have significant medical comorbidities. Common sequelae of bariatric surgery are mineral and nutrient deficiencies. This case highlights how an acquired copper deficiency led to the development of rapidly progressive cirrhosis.
Case Description/Methods: A 54-year-old Latina female with hypertension, hyperlipidemia, Type 2 diabetes mellitus well controlled without medications, and duodenal switch bariatric surgery two years prior presented to our hospital with several week history of weakness, hematochezia, abdominal pain with distension, and jaundice after being referred from clinic for abnormal mixed bilirubinemia. She was diagnosed with cirrhosis with a MELD score of 28 as well as a sideroblastic anemia. Hemochromatosis testing was negative but the liver biopsy revealed an elevated hepatic iron concentration by weight as well as marked macrovesicular steatosis (NAS 8 of 8), bridging fibrosis (Stage 3-4 of 4), prominent Kupffer cells, and hepatocellular hemosiderosis (2-3+). Within a span of a month, she developed hepatorenal syndrome with cirrhosis progression to a MELD of 50. She transitioned to hospice and passed away two weeks later. Notably, her MELD score nine months prior to cirrhosis diagnosis was only 6.
Discussion: This case is unique because the patient developed an acquired copper deficiency secondary to bariatric surgery which caused a rapidly-progressive cirrhosis as is evidenced by the elevated hepatic iron content, extensive hepatic steatosis and fibrosis, presence of sideroblastic anemia, and negative hemochromatosis testing. Copper deficiency prevalence following bariatric surgery is reported to be ~10%.1 Copper deficiency reportedly increases risk of pre-liver transplantation death after adjusting for MELD and comorbidities, likely because it leads to steatohepatitis, iron overload resulting from a secondary ceruloplasmin deficiency, malnutrition, recurrent infections and rarely cirrhosis.2-4 Low copper levels are associated with NAS >5 and significant hepatic ballooning.5 This patient’s duodenal switch surgery significantly increased her risk of copper and other mineral deficiencies because the vast majority of copper absorption takes place in the duodenum and ileum.6 In conclusion, post-bariatric surgery patients should be screened for copper deficiencies and supplemented as needed to mitigate the risk of progression to advanced liver cirrhosis.

Disclosures:
David Twitchell, MD1, Aesha Aboueisha, MD2, Jawairia Memon, MD3. P1307 - Sequelae of Bariatric Surgery: Acquired Copper Deficiency Inducing Rapidly-Progressive Cirrhosis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1UT Health San Antonio, San Antonio, TX; 2University of Texas Health Science Center at San Antonio, San Antonio, TX; 3University of Texas Health Science Center San Antonio, San Antonio, TX
Introduction: Weight-loss, or bariatric, surgery is recommended for patients with BMI >35 or >30 if they have significant medical comorbidities. Common sequelae of bariatric surgery are mineral and nutrient deficiencies. This case highlights how an acquired copper deficiency led to the development of rapidly progressive cirrhosis.
Case Description/Methods: A 54-year-old Latina female with hypertension, hyperlipidemia, Type 2 diabetes mellitus well controlled without medications, and duodenal switch bariatric surgery two years prior presented to our hospital with several week history of weakness, hematochezia, abdominal pain with distension, and jaundice after being referred from clinic for abnormal mixed bilirubinemia. She was diagnosed with cirrhosis with a MELD score of 28 as well as a sideroblastic anemia. Hemochromatosis testing was negative but the liver biopsy revealed an elevated hepatic iron concentration by weight as well as marked macrovesicular steatosis (NAS 8 of 8), bridging fibrosis (Stage 3-4 of 4), prominent Kupffer cells, and hepatocellular hemosiderosis (2-3+). Within a span of a month, she developed hepatorenal syndrome with cirrhosis progression to a MELD of 50. She transitioned to hospice and passed away two weeks later. Notably, her MELD score nine months prior to cirrhosis diagnosis was only 6.
Discussion: This case is unique because the patient developed an acquired copper deficiency secondary to bariatric surgery which caused a rapidly-progressive cirrhosis as is evidenced by the elevated hepatic iron content, extensive hepatic steatosis and fibrosis, presence of sideroblastic anemia, and negative hemochromatosis testing. Copper deficiency prevalence following bariatric surgery is reported to be ~10%.1 Copper deficiency reportedly increases risk of pre-liver transplantation death after adjusting for MELD and comorbidities, likely because it leads to steatohepatitis, iron overload resulting from a secondary ceruloplasmin deficiency, malnutrition, recurrent infections and rarely cirrhosis.2-4 Low copper levels are associated with NAS >5 and significant hepatic ballooning.5 This patient’s duodenal switch surgery significantly increased her risk of copper and other mineral deficiencies because the vast majority of copper absorption takes place in the duodenum and ileum.6 In conclusion, post-bariatric surgery patients should be screened for copper deficiencies and supplemented as needed to mitigate the risk of progression to advanced liver cirrhosis.

Figure: Figure 1: Duodenal Switch Bariatric Surgery Schematic
Source: https://www.nycbariatrics.com/weight-loss-surgery-options/duodenal
Source: https://www.nycbariatrics.com/weight-loss-surgery-options/duodenal
Disclosures:
David Twitchell indicated no relevant financial relationships.
Aesha Aboueisha indicated no relevant financial relationships.
Jawairia Memon indicated no relevant financial relationships.
David Twitchell, MD1, Aesha Aboueisha, MD2, Jawairia Memon, MD3. P1307 - Sequelae of Bariatric Surgery: Acquired Copper Deficiency Inducing Rapidly-Progressive Cirrhosis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
