Sunday Poster Session
Category: Small Intestine
P1314 - Melena and Duodenal Nodule in a Breast Cancer Survivor: A Diagnostic Challenge
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio
- NR
Nikhil Roy Chaudhury, MD
Medical City Fort Worth
Fort Worth, Texas
Presenting Author(s)
Nikhil Roy Chaudhury, MD1, Samiran Roy Chaudhury, MD2, Trina Matthews, DO1, Long T. Hoang, DO3, Monte Troutman, DO4, Joyce Roy, DO1
1Medical City Fort Worth, Fort Worth, TX; 2NYC Health and Hospitals South Brooklyn Health, Staten Island, NY; 3UNT Health, Fort Worth, TX; 4University of North Texas, Fort Worth, TX
Introduction: Neuroendocrine tumors are an uncommon GI pathology that form a small percentage of cancers. Invasive ductal breast carcinomas are more common and can metastasize to bone, lungs and liver but can also less commonly involve the colon and small bowel. A neuroendocrine tumor in the setting of invasive breast cancer is clinically noteworthy and we present a clinical example of such below.
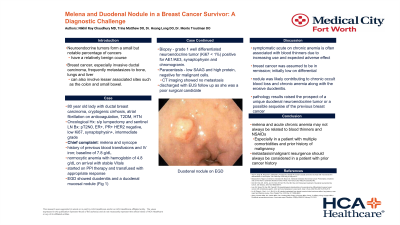
Case Description/Methods: An 80 yo lady, with Hx of invasive ductal breast carcinoma with neuroendocrine features (intermediate grade) s/p lumpectomy and radiation, now in remission [s/p sentinel LN Bx 4/2017 pT2N0, ER+, PR+ HER2 negative, low Ki67, synaptophysin+], cryptogenic cirrhosis, atrial fibrillation on anticoagulation, chronic anemia requiring transfusions presented with syncopal episode and dark tarry stools. She was found to have melena on exam and referred for evaluation. On arrival, she had normocytic anemia with Hb of 4.8 (baseline 7.8). Vitals were stable. PPI therapy was started and transfusion given with appropriate response. Paracentesis was done as patient reported increasing abdominal distention which revealed low SAAG, high protein but no malignant cells. EGD showed duodenitis and a duodenal mucosal nodule. Biopsy showed grade 1 well differentiated neuroendocrine tumor (Ki67 < 1%) positive for AE1/AE3, synaptophysin and chromogranin. CT imaging showed no metastatic lesions and the patient was discharged with follow up for outpatient.
Discussion: Melena and symptomatic anemia are common presentations, especially when associated with blood thinners. Her breast cancer in remission was not a top differential for etiologies. Subsequent pathology of the duodenal nodule raised the prospect of a unique duodenal neuroendocrine tumor as is its own entity vs a possible sequelae of the previous breast cancer. The pathological features of the duodenal nodule are very similar to that of the breast cancer; low ki67 and synaptophysin+ staining. The patient’s cirrhosis and low SAAG ascites also favored malignancy. Pt denied diarrhea, flushing and other Sx related to carcinoid tumor. The nodule was likely contributing to occult blood loss which was contributing to pt’s chronic anemia. In a patient with multiple comorbidities and prior history of malignancy, metastasis/malignant resurgence should always be considered, even if such differentials may not be high on the list.
Disclosures:
Nikhil Roy Chaudhury, MD1, Samiran Roy Chaudhury, MD2, Trina Matthews, DO1, Long T. Hoang, DO3, Monte Troutman, DO4, Joyce Roy, DO1. P1314 - Melena and Duodenal Nodule in a Breast Cancer Survivor: A Diagnostic Challenge, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Medical City Fort Worth, Fort Worth, TX; 2NYC Health and Hospitals South Brooklyn Health, Staten Island, NY; 3UNT Health, Fort Worth, TX; 4University of North Texas, Fort Worth, TX
Introduction: Neuroendocrine tumors are an uncommon GI pathology that form a small percentage of cancers. Invasive ductal breast carcinomas are more common and can metastasize to bone, lungs and liver but can also less commonly involve the colon and small bowel. A neuroendocrine tumor in the setting of invasive breast cancer is clinically noteworthy and we present a clinical example of such below.
Case Description/Methods: An 80 yo lady, with Hx of invasive ductal breast carcinoma with neuroendocrine features (intermediate grade) s/p lumpectomy and radiation, now in remission [s/p sentinel LN Bx 4/2017 pT2N0, ER+, PR+ HER2 negative, low Ki67, synaptophysin+], cryptogenic cirrhosis, atrial fibrillation on anticoagulation, chronic anemia requiring transfusions presented with syncopal episode and dark tarry stools. She was found to have melena on exam and referred for evaluation. On arrival, she had normocytic anemia with Hb of 4.8 (baseline 7.8). Vitals were stable. PPI therapy was started and transfusion given with appropriate response. Paracentesis was done as patient reported increasing abdominal distention which revealed low SAAG, high protein but no malignant cells. EGD showed duodenitis and a duodenal mucosal nodule. Biopsy showed grade 1 well differentiated neuroendocrine tumor (Ki67 < 1%) positive for AE1/AE3, synaptophysin and chromogranin. CT imaging showed no metastatic lesions and the patient was discharged with follow up for outpatient.
Discussion: Melena and symptomatic anemia are common presentations, especially when associated with blood thinners. Her breast cancer in remission was not a top differential for etiologies. Subsequent pathology of the duodenal nodule raised the prospect of a unique duodenal neuroendocrine tumor as is its own entity vs a possible sequelae of the previous breast cancer. The pathological features of the duodenal nodule are very similar to that of the breast cancer; low ki67 and synaptophysin+ staining. The patient’s cirrhosis and low SAAG ascites also favored malignancy. Pt denied diarrhea, flushing and other Sx related to carcinoid tumor. The nodule was likely contributing to occult blood loss which was contributing to pt’s chronic anemia. In a patient with multiple comorbidities and prior history of malignancy, metastasis/malignant resurgence should always be considered, even if such differentials may not be high on the list.
Disclosures:
Nikhil Roy Chaudhury indicated no relevant financial relationships.
Samiran Roy Chaudhury indicated no relevant financial relationships.
Trina Matthews indicated no relevant financial relationships.
Long Hoang indicated no relevant financial relationships.
Monte Troutman indicated no relevant financial relationships.
Joyce Roy indicated no relevant financial relationships.
Nikhil Roy Chaudhury, MD1, Samiran Roy Chaudhury, MD2, Trina Matthews, DO1, Long T. Hoang, DO3, Monte Troutman, DO4, Joyce Roy, DO1. P1314 - Melena and Duodenal Nodule in a Breast Cancer Survivor: A Diagnostic Challenge, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
