Sunday Poster Session
Category: Small Intestine
P1317 - A Case of Post-COVID Eosinophilic Enteritis Presenting as Protein-Losing Enteropathy
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio
- PH
Ping He, MD, PhD
Rutgers Robert Wood Johnson Medical School
New Brunswick, NJ
Presenting Author(s)
Ping N. He, MD, PhD1, Brittany Muhlgeier, MSN, FNP-C2, Mahmoud Ali, MBBCh1, Anish V. Patel, MD1
1Rutgers Robert Wood Johnson Medical School, New Brunswick, NJ; 2Robert Wood Johnson University Hospital, New Brunswick, NJ
Introduction: Eosinophilic enteritis (EE) is a chronic inflammatory disorder characterized by infiltration of eosinophils into the mucosa, submucosa, or muscularis propria. Its prevalence is between 0.5-5 per 100,000 people. The exact cause is unknown, but believed to be a reaction to environmental allergens. Symptoms include abdominal pain, diarrhea, vomiting, weight loss, and anemia. Diffuse mucosal involvement can lead to protein-losing enteropathy (PLE) characterized by hypoproteinemia and edema.
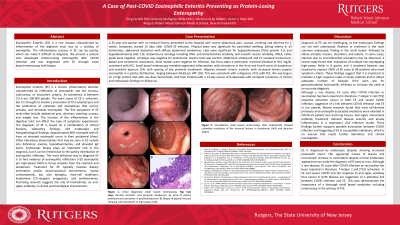
Case Description/Methods: A 35-year-old woman with no medical history presented to the hospital with severe abdominal pain, nausea, vomiting and diarrhea for 2 weeks. Symptoms started 10 days after COVID-19 infection. Physical exam was significant for periorbital swelling, pitting edema in all extremities, abdominal distention with diffuse abdominal tenderness. Labs were significant for hypoproteinemia (Total protein 3.2) and hypoalbuminemia (Alb 1.9). Autoimmune serology including ANA, anti-mitochondrial antibody, anti-smooth muscle antibody, ANCA, celiac panel were negative. Urinalysis was negative for proteinuria. Gastrin level was normal. Abdominal ultrasound and CT revealed normal liver, bowel and mesenteric vasculature. Stool studies were negative for infection, but fecal alpha-1-antitrypsin returned elevated at 916 mg/dL consistent with PLE. Small bowel enteroscopy revealed segmental inflammation with ulcerations in the third and fourth parts of duodenum and proximal jejunum (1A) with sparing of the proximal duodenum. Biopsies showed chronic enteritis with increased lamina propria eosinophils in a patchy distribution, ranging between 30-60 per hpf (1B). This was consistent with a diagnosis of EE with PLE. She was begun on a high protein diet with low dose furosemide. And then treated with a 14-day course of budesonide with complete resolution of clinical and endoscopic findings on followup.
Discussion: EE is diagnosed by endoscopic biopsies showing increased eosinophil count. The segmental nature of lesions and microscopic increase in eosinophils despite normal endoscopic appearance can make the diagnosis of EE easy to miss. Although a rare disease, EE cases after COVID infection or vaccination has been reported in literature. T-Helper 2 cell (Th2) response activation occurs in both EE and severe COVID infection, suggestive of a link between COVID infection and EE in our patient. This case demonstrates the importance of thorough small bowel evaluation including enteroscopy in the workup of PLE.

Disclosures:
Ping N. He, MD, PhD1, Brittany Muhlgeier, MSN, FNP-C2, Mahmoud Ali, MBBCh1, Anish V. Patel, MD1. P1317 - A Case of Post-COVID Eosinophilic Enteritis Presenting as Protein-Losing Enteropathy, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Rutgers Robert Wood Johnson Medical School, New Brunswick, NJ; 2Robert Wood Johnson University Hospital, New Brunswick, NJ
Introduction: Eosinophilic enteritis (EE) is a chronic inflammatory disorder characterized by infiltration of eosinophils into the mucosa, submucosa, or muscularis propria. Its prevalence is between 0.5-5 per 100,000 people. The exact cause is unknown, but believed to be a reaction to environmental allergens. Symptoms include abdominal pain, diarrhea, vomiting, weight loss, and anemia. Diffuse mucosal involvement can lead to protein-losing enteropathy (PLE) characterized by hypoproteinemia and edema.
Case Description/Methods: A 35-year-old woman with no medical history presented to the hospital with severe abdominal pain, nausea, vomiting and diarrhea for 2 weeks. Symptoms started 10 days after COVID-19 infection. Physical exam was significant for periorbital swelling, pitting edema in all extremities, abdominal distention with diffuse abdominal tenderness. Labs were significant for hypoproteinemia (Total protein 3.2) and hypoalbuminemia (Alb 1.9). Autoimmune serology including ANA, anti-mitochondrial antibody, anti-smooth muscle antibody, ANCA, celiac panel were negative. Urinalysis was negative for proteinuria. Gastrin level was normal. Abdominal ultrasound and CT revealed normal liver, bowel and mesenteric vasculature. Stool studies were negative for infection, but fecal alpha-1-antitrypsin returned elevated at 916 mg/dL consistent with PLE. Small bowel enteroscopy revealed segmental inflammation with ulcerations in the third and fourth parts of duodenum and proximal jejunum (1A) with sparing of the proximal duodenum. Biopsies showed chronic enteritis with increased lamina propria eosinophils in a patchy distribution, ranging between 30-60 per hpf (1B). This was consistent with a diagnosis of EE with PLE. She was begun on a high protein diet with low dose furosemide. And then treated with a 14-day course of budesonide with complete resolution of clinical and endoscopic findings on followup.
Discussion: EE is diagnosed by endoscopic biopsies showing increased eosinophil count. The segmental nature of lesions and microscopic increase in eosinophils despite normal endoscopic appearance can make the diagnosis of EE easy to miss. Although a rare disease, EE cases after COVID infection or vaccination has been reported in literature. T-Helper 2 cell (Th2) response activation occurs in both EE and severe COVID infection, suggestive of a link between COVID infection and EE in our patient. This case demonstrates the importance of thorough small bowel evaluation including enteroscopy in the workup of PLE.

Figure: A. Segmental inflammation in the distal duodenum with ulcerations, biopsied on small bowel enteroscopy. B. chronic enteritis with increased lamina propria eosinophils in a patchy distribution, ranging between 30-60 per hpf.
Disclosures:
Ping He indicated no relevant financial relationships.
Brittany Muhlgeier indicated no relevant financial relationships.
Mahmoud Ali indicated no relevant financial relationships.
Anish Patel indicated no relevant financial relationships.
Ping N. He, MD, PhD1, Brittany Muhlgeier, MSN, FNP-C2, Mahmoud Ali, MBBCh1, Anish V. Patel, MD1. P1317 - A Case of Post-COVID Eosinophilic Enteritis Presenting as Protein-Losing Enteropathy, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
