Sunday Poster Session
Category: Small Intestine
P1328 - Presentations of Eosinophilic Gastrointestinal Disease Vary Based on the Mucosal Layer Affected
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Randy Leibowitz, DO
Mount Sinai Morningside and Mount Sinai West
New York, NY
Presenting Author(s)
Randy Leibowitz, DO1, Steven Rodriguez, MD2, Daniela Jodorkovsky, MD3, Brijen Shah, MD4
1Mount Sinai Morningside and Mount Sinai West, New York, NY; 2Mount Sinai Beth Israel, Morningside and West, New York, NY; 3Mount Sinai, New York, NY; 4Icahn School of Medicine at Mount Sinai, New York, NY
Introduction: Eosinophilic gastrointestinal diseases (EGID) have a prevalence of about 5/100,000 cases. All regions of the GI tract can be affected and the presentation differs depending on the region or layer of mucosa affected. We will discuss two cases of EGID whose presentations differ based on the location of eosinophilic infiltration.
Case Description/Methods: A 59-year-old woman with a history of asthma, aspirin exacerbated respiratory disease, and chronic gastritis refractory to PPI BID presented with abdominal pain, vomiting, dysphagia and a 30 lb weight loss over 3 months. Labs were notable for peripheral eosinophilia of 9.4% and a negative infectious workup. Esophagogastroduodenoscopy (EGD) was notable for gastric fundus and duodenal bulb erythema. Pathology was notable for increased eosinophils in the duodenum, gastric body and fundus and esophagus ranging from 31-99 per hpf.
A 33-year-old woman presented with burning epigastric pain, which was worse with eating and associated with abdominal distention. Labs were notable for 57% peripheral eosinophilia and a negative infectious workup. Computed tomography was notable for ascites and bowel wall thickening in the duodenum and colon. Paracentesis showed elevated leukocytes in the ascitic fluid with 78% eosinophils. Biopsies obtained during an EGD were notable for increased eosinophils in duodenum, gastric and esophageal mucosa of 46 per hpf. She required a prolonged prednisone taper and parenteral nutrition. Imaging obtained at the conclusion of the prednisone course showed resolution of bowel wall thickening and ascites.
Discussion: Mucosal disease typically presents with nonspecific symptoms and may result in malabsorption. Muscularis disease can cause impaired motility and stricture formation, resulting in obstruction. Serosal disease may present with ascites with an eosinophilic predominance. Currently, there is no universal diagnostic criteria based on the number of eosinophils seen on endoscopic biopsy.
Conservative treatment includes a six food elimination diet and implementation of an elemental diet. First line therapy includes prednisone 20-40 mg per day for 2 weeks then tapered over 2 weeks or 5-10 mg daily for refractory symptoms. 9 mg daily of budesonide was shown to have a more favorable safety profile compared to prednisone.. Other agents such as cromolyn and biologic agents such as omalizumab, vedolizumab and benralizumab have all been shown to induce histologic remission.

Disclosures:
Randy Leibowitz, DO1, Steven Rodriguez, MD2, Daniela Jodorkovsky, MD3, Brijen Shah, MD4. P1328 - Presentations of Eosinophilic Gastrointestinal Disease Vary Based on the Mucosal Layer Affected, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Mount Sinai Morningside and Mount Sinai West, New York, NY; 2Mount Sinai Beth Israel, Morningside and West, New York, NY; 3Mount Sinai, New York, NY; 4Icahn School of Medicine at Mount Sinai, New York, NY
Introduction: Eosinophilic gastrointestinal diseases (EGID) have a prevalence of about 5/100,000 cases. All regions of the GI tract can be affected and the presentation differs depending on the region or layer of mucosa affected. We will discuss two cases of EGID whose presentations differ based on the location of eosinophilic infiltration.
Case Description/Methods: A 59-year-old woman with a history of asthma, aspirin exacerbated respiratory disease, and chronic gastritis refractory to PPI BID presented with abdominal pain, vomiting, dysphagia and a 30 lb weight loss over 3 months. Labs were notable for peripheral eosinophilia of 9.4% and a negative infectious workup. Esophagogastroduodenoscopy (EGD) was notable for gastric fundus and duodenal bulb erythema. Pathology was notable for increased eosinophils in the duodenum, gastric body and fundus and esophagus ranging from 31-99 per hpf.
A 33-year-old woman presented with burning epigastric pain, which was worse with eating and associated with abdominal distention. Labs were notable for 57% peripheral eosinophilia and a negative infectious workup. Computed tomography was notable for ascites and bowel wall thickening in the duodenum and colon. Paracentesis showed elevated leukocytes in the ascitic fluid with 78% eosinophils. Biopsies obtained during an EGD were notable for increased eosinophils in duodenum, gastric and esophageal mucosa of 46 per hpf. She required a prolonged prednisone taper and parenteral nutrition. Imaging obtained at the conclusion of the prednisone course showed resolution of bowel wall thickening and ascites.
Discussion: Mucosal disease typically presents with nonspecific symptoms and may result in malabsorption. Muscularis disease can cause impaired motility and stricture formation, resulting in obstruction. Serosal disease may present with ascites with an eosinophilic predominance. Currently, there is no universal diagnostic criteria based on the number of eosinophils seen on endoscopic biopsy.
Conservative treatment includes a six food elimination diet and implementation of an elemental diet. First line therapy includes prednisone 20-40 mg per day for 2 weeks then tapered over 2 weeks or 5-10 mg daily for refractory symptoms. 9 mg daily of budesonide was shown to have a more favorable safety profile compared to prednisone.. Other agents such as cromolyn and biologic agents such as omalizumab, vedolizumab and benralizumab have all been shown to induce histologic remission.

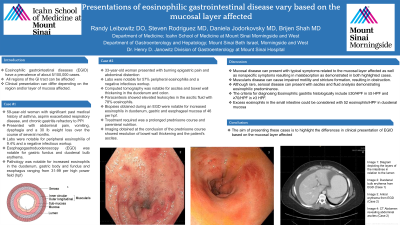
Figure: Image 1: Duodenal bulb erythema from the EGD in case 1
Image 2: Antral erythema from the EGD in case 2
Image 3: CT Abdomen revealing abdominal ascites in case 2
Image 2: Antral erythema from the EGD in case 2
Image 3: CT Abdomen revealing abdominal ascites in case 2
Disclosures:
Randy Leibowitz indicated no relevant financial relationships.
Steven Rodriguez indicated no relevant financial relationships.
Daniela Jodorkovsky: ATMO Biosciences – Consultant.
Brijen Shah indicated no relevant financial relationships.
Randy Leibowitz, DO1, Steven Rodriguez, MD2, Daniela Jodorkovsky, MD3, Brijen Shah, MD4. P1328 - Presentations of Eosinophilic Gastrointestinal Disease Vary Based on the Mucosal Layer Affected, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

