Sunday Poster Session
Category: Stomach
P1341 - Positive Association of Dietary Salt Intake and Gastric Intestinal Metaplasia: A Systematic Review and Meta-analysis
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Eleazar E. Montalvan-Sanchez, MD
Indiana University School of Medicine
Indianapolis, IN
Presenting Author(s)
Eleazar E.. Montalvan-Sanchez, MD1, Dalton A. Norwood, MD2, Diego Izquierdo-Veraza, MD1, Blanca Estefanie. Avalos-Quijano, MS3, Renato Beas, MD4, Mirian Ramirez-Rojas, MLIS5, Aida Rodriguez-Murillo, MD1, Bernardo Donery Lopez Samayoa, MD6, Tatiana Torres Herman, MD7, Douglas Morgan, MD, MPH7
1Indiana University School of Medicine, Indianapolis, IN; 2UAB Minority Health and Health Equity Research Center, The University of Alabama at Birmingham Heersink School of Medicine, Birmingham, AL; 3Universidad Evangélica de El Salvador, Wilmington, NC; 4Indiana University, Indianapolis, IN; 5Ruth Lilly Medical Library, Indiana University School of Medicine, Indianapolis, IN; 6Johns Hopkins Bloomberg School of Public Health, San Bernardino, CA; 7University of Alabama at Birmingham, Birmingham, AL
Introduction: Gastric cancer (GC) is the fourth leading cause of global cancer mortality. Gastric intestinal metaplasia (GIM) is the principal gastric premalignant condition (GPMC) and thought to represent an irreversible histologic point of no return. Dietary salt intake is associated with gastric cancer and is implicated in GIM development and progression. Salt has several carcinogenic effects: the generation of N-nitroso compounds; degradation of the mucosal barrier with inflammation; and increased colonization and inflammation by H. pylori, particularly cagA+ strains. We performed a systematic review and meta-analysis on the association of salt intake and GIM prevalence.
Methods: We used the PubMed Scopus and Web of Science databases, with the PRISMA protocol, through April 2023 to identify epidemiological studies published in English assessing the association of salt consumption and the GIM prevalence. Two independent reviewers assessed study quality/risk for bias using Newcastle-Ottawa Scale (NOS) and extracted descriptive and quantitative data. The pooled OR estimates were calculated, heterogeneity was assessed by the inconsistency index (I2).
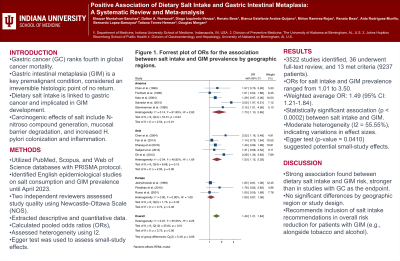
Results: The literature search yielded 3522 studies, of which 36 were identified for full-text review, with 13 studies filling the criteria for final analysis including 9237 patients. The odds ratios (ORs) for the association between salt intake and GIM prevalence ranged from 1.01 to 3.50 across the included studies. The weighted average OR was 1.49 (95%; 1.21-1.84). The test of theta (= 0) z-value was 3.75, demonstrating a statistically significant association between salt intake and GIM (p < 0.0002). The heterogeneity analysis revealed a moderate level of heterogeneity, with an I2 value of 55.55%, indicating variations in effect sizes across the studies. The regression-based Egger test (p-value =0.0410) implied potential small-study effects in our meta-analysis.
Discussion: Our findings suggest an association between dietary salt intake and the risk of developing GIM. The association was stronger than that observed in studies with GC as the endpoint. There was no significant difference by geographic region nor by the study design. Salt intake recommendations should be included in overall risk-reduction recommendations (e.g., tobacco, alcohol) in patients with GIM.

Disclosures:
Eleazar E.. Montalvan-Sanchez, MD1, Dalton A. Norwood, MD2, Diego Izquierdo-Veraza, MD1, Blanca Estefanie. Avalos-Quijano, MS3, Renato Beas, MD4, Mirian Ramirez-Rojas, MLIS5, Aida Rodriguez-Murillo, MD1, Bernardo Donery Lopez Samayoa, MD6, Tatiana Torres Herman, MD7, Douglas Morgan, MD, MPH7. P1341 - Positive Association of Dietary Salt Intake and Gastric Intestinal Metaplasia: A Systematic Review and Meta-analysis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Indiana University School of Medicine, Indianapolis, IN; 2UAB Minority Health and Health Equity Research Center, The University of Alabama at Birmingham Heersink School of Medicine, Birmingham, AL; 3Universidad Evangélica de El Salvador, Wilmington, NC; 4Indiana University, Indianapolis, IN; 5Ruth Lilly Medical Library, Indiana University School of Medicine, Indianapolis, IN; 6Johns Hopkins Bloomberg School of Public Health, San Bernardino, CA; 7University of Alabama at Birmingham, Birmingham, AL
Introduction: Gastric cancer (GC) is the fourth leading cause of global cancer mortality. Gastric intestinal metaplasia (GIM) is the principal gastric premalignant condition (GPMC) and thought to represent an irreversible histologic point of no return. Dietary salt intake is associated with gastric cancer and is implicated in GIM development and progression. Salt has several carcinogenic effects: the generation of N-nitroso compounds; degradation of the mucosal barrier with inflammation; and increased colonization and inflammation by H. pylori, particularly cagA+ strains. We performed a systematic review and meta-analysis on the association of salt intake and GIM prevalence.
Methods: We used the PubMed Scopus and Web of Science databases, with the PRISMA protocol, through April 2023 to identify epidemiological studies published in English assessing the association of salt consumption and the GIM prevalence. Two independent reviewers assessed study quality/risk for bias using Newcastle-Ottawa Scale (NOS) and extracted descriptive and quantitative data. The pooled OR estimates were calculated, heterogeneity was assessed by the inconsistency index (I2).
Results: The literature search yielded 3522 studies, of which 36 were identified for full-text review, with 13 studies filling the criteria for final analysis including 9237 patients. The odds ratios (ORs) for the association between salt intake and GIM prevalence ranged from 1.01 to 3.50 across the included studies. The weighted average OR was 1.49 (95%; 1.21-1.84). The test of theta (= 0) z-value was 3.75, demonstrating a statistically significant association between salt intake and GIM (p < 0.0002). The heterogeneity analysis revealed a moderate level of heterogeneity, with an I2 value of 55.55%, indicating variations in effect sizes across the studies. The regression-based Egger test (p-value =0.0410) implied potential small-study effects in our meta-analysis.
Discussion: Our findings suggest an association between dietary salt intake and the risk of developing GIM. The association was stronger than that observed in studies with GC as the endpoint. There was no significant difference by geographic region nor by the study design. Salt intake recommendations should be included in overall risk-reduction recommendations (e.g., tobacco, alcohol) in patients with GIM.

Figure: Forrest plot of ORs for the association between salt intake and GIM prevalence by geographic regions.
Disclosures:
Eleazar Montalvan-Sanchez indicated no relevant financial relationships.
Dalton Norwood indicated no relevant financial relationships.
Diego Izquierdo-Veraza indicated no relevant financial relationships.
Blanca Avalos-Quijano indicated no relevant financial relationships.
Renato Beas indicated no relevant financial relationships.
Mirian Ramirez-Rojas indicated no relevant financial relationships.
Aida Rodriguez-Murillo indicated no relevant financial relationships.
Bernardo Donery Lopez Samayoa indicated no relevant financial relationships.
Tatiana Torres Herman indicated no relevant financial relationships.
Douglas Morgan: American Molecular Laboratory – Investigator initiated study, company donated analysis. CDx Diagnostics – Investigator initiated study, company donated analysis. Panbela Therapeutics – NCI-funded study, company donated study drug to the University. Thorne – NCI-funded study, company donated study drug to the University.
Eleazar E.. Montalvan-Sanchez, MD1, Dalton A. Norwood, MD2, Diego Izquierdo-Veraza, MD1, Blanca Estefanie. Avalos-Quijano, MS3, Renato Beas, MD4, Mirian Ramirez-Rojas, MLIS5, Aida Rodriguez-Murillo, MD1, Bernardo Donery Lopez Samayoa, MD6, Tatiana Torres Herman, MD7, Douglas Morgan, MD, MPH7. P1341 - Positive Association of Dietary Salt Intake and Gastric Intestinal Metaplasia: A Systematic Review and Meta-analysis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
