Sunday Poster Session
Category: Stomach
P1349 - Yellow Granules: An Unusual Case of Gastritis
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio
- MY
Megan Yeager, MSN, RN, CRNP
WellSpan
Lebanon, Pennsylvania
Presenting Author(s)
Megan Yeager, MSN, RN, CRNP, Iryna Hepburn, MD, FACG
WellSpan, Lebanon, PA
Introduction: Actinomyces are G-positive anaerobes that rarely cause chronic granulomatous gastritis. It is rare in the GI tract due to the low gastric pH. We present a patient who was diagnosed with actinomycosis gastritis after 1 year of nausea and vomiting.
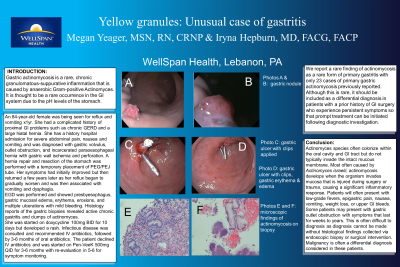
Case Description/Methods: Patient is an 84yo female with long history of chronic GERD and large hiatal hernia. 4 years ago she presented with abdominal pain, nausea and vomiting, was diagnosed with gastric volvulus, outlet obstruction, incarcerated paraesophageal hernia with ischemia and perforation. Hernia repair, gastric resection, and temporary PEG/PEJ were performed, and her symptoms improved but returned 1 year later. EGD showed gastritis, erosions and multiple ulcerations with mild bleeding. Gastric biopsies revealed active gastritis and clumps of actinomyces. She was given doxycycline 100mg twice daily but developed a rash. Infectious disease was consulted, and treatment with IV penicillin followed by 3-6 months of oral penicillin was recommended. Patient had declined initiation of intravenous antibiotics and was treated with oral Pen-Vee K 500mg with a plan for re-evaluation in 5-6 weeks.
Discussion: Actinomycosis is a rare form of gastritis with only 23 cases of primary gastric actinomycosis reported. Actinomyces often colonize oral cavity and GI tract but do not typically invade the intact mucous membrane. Most often caused by Actinomyces israelii, actinomycosis develops when organism invades mucosa injured during surgery or trauma, causing significant inflammatory response. Patients usually presents with fevers, epigastric pain, nausea, vomiting, weight loss, or GI bleed. Some patients may present with gastric outlet obstruction with symptoms lasting anywhere from a few weeks to years. Due to similar presentation, malignancy is often considered in differential. Diagnosis can be difficult and requires tissue sampling, endoscopy or surgical intervention. Uncomplicated actinomycosis is typically treated with a course of IV penicillin, followed by oral penicillin for 3-12 months. Surgical intervention is reserved for cases of obstruction or failure to respond to antibiotics. After surgery, a much shorter course of antibiotics is needed, especially if the entire cite of actinomycosis was removed.
In conclusion, actinomycosis is a rare cause of gastritis, it should be considered in patients with prior history of GI surgery who experience persistent symptoms so diagnostic investigation is undertaken and appropriate treatment is initiated.
Disclosures:
Megan Yeager, MSN, RN, CRNP, Iryna Hepburn, MD, FACG. P1349 - Yellow Granules: An Unusual Case of Gastritis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
WellSpan, Lebanon, PA
Introduction: Actinomyces are G-positive anaerobes that rarely cause chronic granulomatous gastritis. It is rare in the GI tract due to the low gastric pH. We present a patient who was diagnosed with actinomycosis gastritis after 1 year of nausea and vomiting.
Case Description/Methods: Patient is an 84yo female with long history of chronic GERD and large hiatal hernia. 4 years ago she presented with abdominal pain, nausea and vomiting, was diagnosed with gastric volvulus, outlet obstruction, incarcerated paraesophageal hernia with ischemia and perforation. Hernia repair, gastric resection, and temporary PEG/PEJ were performed, and her symptoms improved but returned 1 year later. EGD showed gastritis, erosions and multiple ulcerations with mild bleeding. Gastric biopsies revealed active gastritis and clumps of actinomyces. She was given doxycycline 100mg twice daily but developed a rash. Infectious disease was consulted, and treatment with IV penicillin followed by 3-6 months of oral penicillin was recommended. Patient had declined initiation of intravenous antibiotics and was treated with oral Pen-Vee K 500mg with a plan for re-evaluation in 5-6 weeks.
Discussion: Actinomycosis is a rare form of gastritis with only 23 cases of primary gastric actinomycosis reported. Actinomyces often colonize oral cavity and GI tract but do not typically invade the intact mucous membrane. Most often caused by Actinomyces israelii, actinomycosis develops when organism invades mucosa injured during surgery or trauma, causing significant inflammatory response. Patients usually presents with fevers, epigastric pain, nausea, vomiting, weight loss, or GI bleed. Some patients may present with gastric outlet obstruction with symptoms lasting anywhere from a few weeks to years. Due to similar presentation, malignancy is often considered in differential. Diagnosis can be difficult and requires tissue sampling, endoscopy or surgical intervention. Uncomplicated actinomycosis is typically treated with a course of IV penicillin, followed by oral penicillin for 3-12 months. Surgical intervention is reserved for cases of obstruction or failure to respond to antibiotics. After surgery, a much shorter course of antibiotics is needed, especially if the entire cite of actinomycosis was removed.
In conclusion, actinomycosis is a rare cause of gastritis, it should be considered in patients with prior history of GI surgery who experience persistent symptoms so diagnostic investigation is undertaken and appropriate treatment is initiated.
Disclosures:
Megan Yeager indicated no relevant financial relationships.
Iryna Hepburn indicated no relevant financial relationships.
Megan Yeager, MSN, RN, CRNP, Iryna Hepburn, MD, FACG. P1349 - Yellow Granules: An Unusual Case of Gastritis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
