Sunday Poster Session
Category: Stomach
P1358 - Spontaneous Regression of a Rare Gastric Epstein-Barr Virus-Positive Mucocutaneous Ulcer, an Entity in Age-Related Immunosenescence
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Rita Auro, MD
Cooper University Health Care
Camden, NJ
Presenting Author(s)
Rita Auro, MD, Jason Ho, MD, Apeksha Shah, MD
Cooper University Health Care, Camden, NJ
Introduction: Epstein-Barr virus-positive mucocutaneous ulcer (EBVMCU) is a lymphoproliferative disorder characterized by skin, oral mucosa, and/or gastrointestinal (GI) tract ulcers. It is associated with various forms of immunosuppression due to reduced T-cells needed to target EBV-associated antigens. It is relatively self-limited, though aggressive lesions have been reported. The lack of standardized diagnostic criteria leaves many questions unanswered regarding management. Here we present a case of gastric EBVMCU which regressed without treatment.
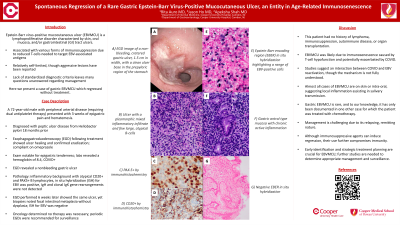
Case Description/Methods: A 72-year-old male with peripheral arterial disease (requiring dual antiplatelet therapy) presented with 3 weeks of epigastric pain and hematemesis. He was diagnosed with peptic ulcer disease from Heliobacter pylori 18 months prior, yet esophagogastroduodenoscopy (EGD) following treatment showed ulcer healing and confirmed eradication. He was compliant on omeprazole. Exam was notable for epigastric tenderness and labs revealed a hemoglobin of 8.4. He was also found to be COVID positive. EGD was performed due to concerns for a GI bleed, which revealed a nonbleeding gastric ulcer. Pathology showed an inflammatory background with atypical CD20+ and PAX5+ B lymphocytes. In situ hybridization (ISH) for EBV was positive. IgH and clonal IgK gene rearrangements were not detected. EGD performed 6 weeks later to evaluate for healing showed the same ulcer, yet biopsies noted focal intestinal metaplasia without dysplasia. ISH for EBV was negative. Oncology determined no therapy was necessary; periodic EGDs were recommended for surveillance.
Discussion: This patient had no history of lymphoma, immunosuppression, autoimmune disease, or organ transplant. EBVMCU was likely due to immunosenescence caused by T-cell hypofunction and potentially exacerbated by COVID. Studies suggest an interaction between COVID and EBV reactivation, though the mechanism is not fully understood. Almost all cases of EBVMCU are on skin or intra-oral, suggesting local inflammation assisting in salivary transmission. Gastric EBVMCU is rare, and to our knowledge, it has only been documented in one other case for which the patient was treated with chemotherapy. Management is challenging due to its relapsing, remitting nature. Although immunosuppressive agents can induce regression, their use further compromises immunity. Early identification and strategic treatment planning are crucial for EBVMCU; further studies are needed to determine appropriate management and surveillance.

Disclosures:
Rita Auro, MD, Jason Ho, MD, Apeksha Shah, MD. P1358 - Spontaneous Regression of a Rare Gastric Epstein-Barr Virus-Positive Mucocutaneous Ulcer, an Entity in Age-Related Immunosenescence, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Cooper University Health Care, Camden, NJ
Introduction: Epstein-Barr virus-positive mucocutaneous ulcer (EBVMCU) is a lymphoproliferative disorder characterized by skin, oral mucosa, and/or gastrointestinal (GI) tract ulcers. It is associated with various forms of immunosuppression due to reduced T-cells needed to target EBV-associated antigens. It is relatively self-limited, though aggressive lesions have been reported. The lack of standardized diagnostic criteria leaves many questions unanswered regarding management. Here we present a case of gastric EBVMCU which regressed without treatment.
Case Description/Methods: A 72-year-old male with peripheral arterial disease (requiring dual antiplatelet therapy) presented with 3 weeks of epigastric pain and hematemesis. He was diagnosed with peptic ulcer disease from Heliobacter pylori 18 months prior, yet esophagogastroduodenoscopy (EGD) following treatment showed ulcer healing and confirmed eradication. He was compliant on omeprazole. Exam was notable for epigastric tenderness and labs revealed a hemoglobin of 8.4. He was also found to be COVID positive. EGD was performed due to concerns for a GI bleed, which revealed a nonbleeding gastric ulcer. Pathology showed an inflammatory background with atypical CD20+ and PAX5+ B lymphocytes. In situ hybridization (ISH) for EBV was positive. IgH and clonal IgK gene rearrangements were not detected. EGD performed 6 weeks later to evaluate for healing showed the same ulcer, yet biopsies noted focal intestinal metaplasia without dysplasia. ISH for EBV was negative. Oncology determined no therapy was necessary; periodic EGDs were recommended for surveillance.
Discussion: This patient had no history of lymphoma, immunosuppression, autoimmune disease, or organ transplant. EBVMCU was likely due to immunosenescence caused by T-cell hypofunction and potentially exacerbated by COVID. Studies suggest an interaction between COVID and EBV reactivation, though the mechanism is not fully understood. Almost all cases of EBVMCU are on skin or intra-oral, suggesting local inflammation assisting in salivary transmission. Gastric EBVMCU is rare, and to our knowledge, it has only been documented in one other case for which the patient was treated with chemotherapy. Management is challenging due to its relapsing, remitting nature. Although immunosuppressive agents can induce regression, their use further compromises immunity. Early identification and strategic treatment planning are crucial for EBVMCU; further studies are needed to determine appropriate management and surveillance.

Figure: A. EGD image of a non-bleeding, cratered gastric ulcer, 1.5 cm in width, with a clean ulcer base (Forrest Class III) in the prepyloric region of the stomach. Mild congestion and erythema noted at ulcer edges. B. Ulcer with a pleomorphic mixed inflammatory infiltrate and few large, atypical B-cells. C. PAX-5+ by immunohistochemistry. D. CD20+ by immunohistochemistry. E. Epstein-Barr encoding region (EBER) in situ hybridization highlighting a range of EBV-positive cells. F. Gastric antral type mucosa with chronic active inflammation. G. Negative EBER in situ hybridization.
Disclosures:
Rita Auro indicated no relevant financial relationships.
Jason Ho indicated no relevant financial relationships.
Apeksha Shah indicated no relevant financial relationships.
Rita Auro, MD, Jason Ho, MD, Apeksha Shah, MD. P1358 - Spontaneous Regression of a Rare Gastric Epstein-Barr Virus-Positive Mucocutaneous Ulcer, an Entity in Age-Related Immunosenescence, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

