Sunday Poster Session
Category: Stomach
P1359 - When Looking at the Stomach Makes It Bleed: A Very Rare Case of Limited Gastric Amyloidosis
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio
- PY
Pradeep Yarra, MD, MSc
Saint Louis University Hospital
St. Louis, MO
Presenting Author(s)
Pradeep Yarra, MD, MSc1, Gebran Khneizer, MD1, Mahmoud Y. Madi, MD1, Danielle Carpenter, MD1, Wissam Kiwan, MD2
1Saint Louis University Hospital, St. Louis, MO; 2Saint Louis University, St. Louis, MO
Introduction: Gastrointestinal amyloidosis has an incidence of 3% of all cases of amyloidosis, is less common with light chain amyloidosis (AL), and even rarer to be localized to single organ without extraintestinal or an associated plasma dyscrasia. Localized Gastric Amyloidosis (LGA) is rare. We present this unique case of recurrent GI bleed due to unusual mucosal hemorrhage that could be triggered by gastric insufflation during endoscopy.
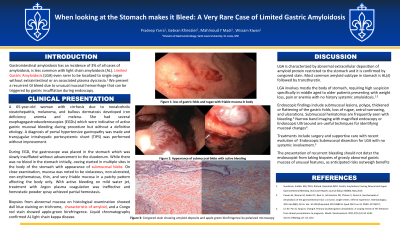
Case Description/Methods: A 65-year-old woman with cirrhosis due to nonalcoholic steatohepatitis, melanoma, and bullous dermatosis developed iron deficiency anemia and melena. She had several esophagogastroduodenoscopies (EGDs) which revealed active gastric mucosal bleeding during procedure but without a definitive etiology. A diagnosis of portal hypertensive gastropathy was made and transjugular intrahepatic portosystemic shunt (TIPS) was placed without improvement. She returned with hematemesis, and an EGD was performed. The gastroscope was placed in the stomach which was slowly insufflated without advancement to the duodenum. While there was no blood in the stomach initially, oozing started in multiple sites in the body of the stomach with appearance of submucosal blebs which were also observed in previous EGDs. The mucosa was closely examined showing a violaceous, non-ulcerated, non-erythematous, thin, and very friable mucosa in a patchy pattern affecting the gastric body. Even mild water jet caused bleeding, while a powerful water jet in normally appearing mucosa caused no bleeding. Argon plasma coagulation was ineffective and hemostatic powder spray achieved partial hemostasis. Biopsies were taken from abnormal mucosa which could slough out easily. On biopsy, there was a dull blue staining on trichrome characteristic of amyloid, and a Congo red stain showed apple-green birefringence. Liquid chromatography confirmed AL light chain kappa disease. Colonoscopy, bone marrow biopsy and positron emission tomography were negative for other organ involvement. She is currently considering treatment options for AL.
Discussion: LGA involves mostly the body of stomach and requires high suspicion specifically in patients with no history systemic amyloidosis. Endoscopic findings include submucosal lesions, polyps, thickened or flattening of the gastric folds, antral narrowing, and ulcerations. Submucosal hematomas are frequently seen. The presentation of recurrent bleeding should not deter the endoscopist from taking biopsies of grossly abnormal gastric mucosa of unusual features.

Disclosures:
Pradeep Yarra, MD, MSc1, Gebran Khneizer, MD1, Mahmoud Y. Madi, MD1, Danielle Carpenter, MD1, Wissam Kiwan, MD2. P1359 - When Looking at the Stomach Makes It Bleed: A Very Rare Case of Limited Gastric Amyloidosis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Saint Louis University Hospital, St. Louis, MO; 2Saint Louis University, St. Louis, MO
Introduction: Gastrointestinal amyloidosis has an incidence of 3% of all cases of amyloidosis, is less common with light chain amyloidosis (AL), and even rarer to be localized to single organ without extraintestinal or an associated plasma dyscrasia. Localized Gastric Amyloidosis (LGA) is rare. We present this unique case of recurrent GI bleed due to unusual mucosal hemorrhage that could be triggered by gastric insufflation during endoscopy.
Case Description/Methods: A 65-year-old woman with cirrhosis due to nonalcoholic steatohepatitis, melanoma, and bullous dermatosis developed iron deficiency anemia and melena. She had several esophagogastroduodenoscopies (EGDs) which revealed active gastric mucosal bleeding during procedure but without a definitive etiology. A diagnosis of portal hypertensive gastropathy was made and transjugular intrahepatic portosystemic shunt (TIPS) was placed without improvement. She returned with hematemesis, and an EGD was performed. The gastroscope was placed in the stomach which was slowly insufflated without advancement to the duodenum. While there was no blood in the stomach initially, oozing started in multiple sites in the body of the stomach with appearance of submucosal blebs which were also observed in previous EGDs. The mucosa was closely examined showing a violaceous, non-ulcerated, non-erythematous, thin, and very friable mucosa in a patchy pattern affecting the gastric body. Even mild water jet caused bleeding, while a powerful water jet in normally appearing mucosa caused no bleeding. Argon plasma coagulation was ineffective and hemostatic powder spray achieved partial hemostasis. Biopsies were taken from abnormal mucosa which could slough out easily. On biopsy, there was a dull blue staining on trichrome characteristic of amyloid, and a Congo red stain showed apple-green birefringence. Liquid chromatography confirmed AL light chain kappa disease. Colonoscopy, bone marrow biopsy and positron emission tomography were negative for other organ involvement. She is currently considering treatment options for AL.
Discussion: LGA involves mostly the body of stomach and requires high suspicion specifically in patients with no history systemic amyloidosis. Endoscopic findings include submucosal lesions, polyps, thickened or flattening of the gastric folds, antral narrowing, and ulcerations. Submucosal hematomas are frequently seen. The presentation of recurrent bleeding should not deter the endoscopist from taking biopsies of grossly abnormal gastric mucosa of unusual features.

Figure: A. First site of spontaneous bleeding in distal body, B. Friable irregular mucosa in proximal body post insufflation, C. Submucosal blebs
Disclosures:
Pradeep Yarra indicated no relevant financial relationships.
Gebran Khneizer indicated no relevant financial relationships.
Mahmoud Madi indicated no relevant financial relationships.
Danielle Carpenter indicated no relevant financial relationships.
Wissam Kiwan indicated no relevant financial relationships.
Pradeep Yarra, MD, MSc1, Gebran Khneizer, MD1, Mahmoud Y. Madi, MD1, Danielle Carpenter, MD1, Wissam Kiwan, MD2. P1359 - When Looking at the Stomach Makes It Bleed: A Very Rare Case of Limited Gastric Amyloidosis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
