Sunday Poster Session
Category: Stomach
P1401 - Emphysematous Gastritis in Multiple Sclerosis: A Rare Presentation
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Tanisha Kalra, MD
SUNY Downstate Health Sciences University/NYCHHC Kings County Hospital
New York, NY
Presenting Author(s)
Tanisha Kalra, MD1, Nikhita Kalra, 2, Kakin R.. Iong, MD3
1SUNY Downstate Health Sciences University/NYCHHC Kings County Hospital, New York, NY; 2Maulana Azad Medical College, New Delhi, Delhi, India; 3SUNY Downstate Health Sciences University, New York, NY
Introduction: Emphysematous gastritis (EG) is a rare life-threatening condition caused by gas-producing microorganisms (like Escherichia coli, Enterobacter, Clostridium, Pseudomonas aeruginosa) and characterized by air in the gastric wall. Predisposing risk factors are alcohol use, diabetes mellitus, renal failure, recent abdominal surgery, gastroenteritis, steroids, and corrosive ingestion. We present a case of EG in a patient with multiple sclerosis (MS).
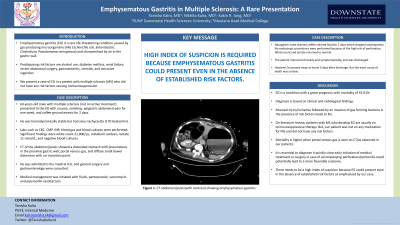
Case Description/Methods: A 64-years-old male with multiple sclerosis (not on active treatment) presented to the ED with nausea, vomiting, epigastric abdominal pain for one week, and coffee-ground emesis for 2 days. He was hemodynamically stable but had sinus tachycardia (170 beats/min). Labs such as CBC, CMP, INR, blood gas and blood cultures were performed. Significant findings were white count 21,000/µL, metabolic acidosis, lactate 11 mmol/L, and negative blood cultures. CT of the abdomen/pelvis showed a distended stomach with pneumatosis in the proximal gastric wall, portal venous gas, and diffuse small bowel distension with no transition point. He was admitted to the medical ICU, and general surgery and gastroenterology were consulted. Medical management was initiated with fluids, pantoprazole, vancomycin and piperacillin-tazobactum. Nasogastric tube drained coffee-colored fluid for 2 days which stopped subsequently. No endoscopic procedures were performed because of the high risk of perforation. White count and lactate returned to normal. The patient improved clinically and symptomatically, and was discharged. However, he passed away at home 5 days after discharge. But the exact cause of death was unclear.
Discussion: EG is a condition with a grave prognosis with mortality of 55-61%. Diagnosis is based on clinical and radiological findings. Mucosal injury/ischemia followed by an invasion of gas forming bacteria in the presence of risk factors leads to EG. On literature review, patients with MS who develop EG are usually on immunosuppressive therapy. But, our patient was not on any medication for MS and did not have any risk factors. Mortality is higher when portal venous gas is seen on CT(as observed in our patient). It is essential to diagnose it quickly since early initiation of medical treatment or surgery in case of accompanying perforation/peritonitis could potentially lead to a more favorable outcome. There needs to be a high index of suspicion because EG could present even in the absence of established risk factors as emphasized by our case.

Disclosures:
Tanisha Kalra, MD1, Nikhita Kalra, 2, Kakin R.. Iong, MD3. P1401 - Emphysematous Gastritis in Multiple Sclerosis: A Rare Presentation, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1SUNY Downstate Health Sciences University/NYCHHC Kings County Hospital, New York, NY; 2Maulana Azad Medical College, New Delhi, Delhi, India; 3SUNY Downstate Health Sciences University, New York, NY
Introduction: Emphysematous gastritis (EG) is a rare life-threatening condition caused by gas-producing microorganisms (like Escherichia coli, Enterobacter, Clostridium, Pseudomonas aeruginosa) and characterized by air in the gastric wall. Predisposing risk factors are alcohol use, diabetes mellitus, renal failure, recent abdominal surgery, gastroenteritis, steroids, and corrosive ingestion. We present a case of EG in a patient with multiple sclerosis (MS).
Case Description/Methods: A 64-years-old male with multiple sclerosis (not on active treatment) presented to the ED with nausea, vomiting, epigastric abdominal pain for one week, and coffee-ground emesis for 2 days. He was hemodynamically stable but had sinus tachycardia (170 beats/min). Labs such as CBC, CMP, INR, blood gas and blood cultures were performed. Significant findings were white count 21,000/µL, metabolic acidosis, lactate 11 mmol/L, and negative blood cultures. CT of the abdomen/pelvis showed a distended stomach with pneumatosis in the proximal gastric wall, portal venous gas, and diffuse small bowel distension with no transition point. He was admitted to the medical ICU, and general surgery and gastroenterology were consulted. Medical management was initiated with fluids, pantoprazole, vancomycin and piperacillin-tazobactum. Nasogastric tube drained coffee-colored fluid for 2 days which stopped subsequently. No endoscopic procedures were performed because of the high risk of perforation. White count and lactate returned to normal. The patient improved clinically and symptomatically, and was discharged. However, he passed away at home 5 days after discharge. But the exact cause of death was unclear.
Discussion: EG is a condition with a grave prognosis with mortality of 55-61%. Diagnosis is based on clinical and radiological findings. Mucosal injury/ischemia followed by an invasion of gas forming bacteria in the presence of risk factors leads to EG. On literature review, patients with MS who develop EG are usually on immunosuppressive therapy. But, our patient was not on any medication for MS and did not have any risk factors. Mortality is higher when portal venous gas is seen on CT(as observed in our patient). It is essential to diagnose it quickly since early initiation of medical treatment or surgery in case of accompanying perforation/peritonitis could potentially lead to a more favorable outcome. There needs to be a high index of suspicion because EG could present even in the absence of established risk factors as emphasized by our case.

Figure: CT abdomen/pelvis(with contrast) showing emphysematous gastritis
Disclosures:
Tanisha Kalra indicated no relevant financial relationships.
Nikhita Kalra indicated no relevant financial relationships.
Kakin Iong indicated no relevant financial relationships.
Tanisha Kalra, MD1, Nikhita Kalra, 2, Kakin R.. Iong, MD3. P1401 - Emphysematous Gastritis in Multiple Sclerosis: A Rare Presentation, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
