Sunday Poster Session
Category: Stomach
P1407 - Cocaine-Induced Gastric Ulcers: An Under-Recognized Disease
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Aakhila Rameeza, DO
Cooper University Hospital
Camden, NJ
Presenting Author(s)
Aakhila Rameeza, DO1, Avneet Singh, DO1, Alexander Garcia, DO1, Peter Bross, MD1, Adib Chaaya, MD2
1Cooper University Hospital, Camden, NJ; 2Cooper Medical School, Camden, NJ
Introduction: In the US, approximately 1.4 million people are affected by cocaine use disorder (CUD). Among the complications of CUD, gastric ulcer formation is less commonly identified since patients often present only after ulcer perforation. As such, gross recognition of cocaine-induced gastric ulcers often goes under recognized. Here we present the case of a patient who was found to have cocaine-induced gastric ulcers on upper endoscopy.
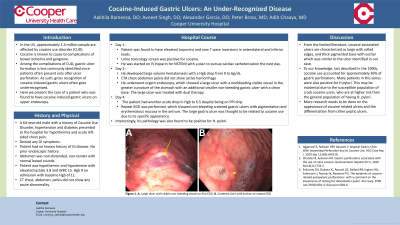
Case Description/Methods: A 64-year-old male with a history of CUD, hypertension and diabetes presented to the hospital for acute left-sided chest pain. He was found to have elevated troponins and new T wave inversions in anterolateral and inferior leads. Urine toxicology screen was positive for cocaine. He was started on IV heparin for NSTEMI with a plan to pursue cardiac catheterization the next day. Subsequently, he developed large volume hematemesis with a Hgb drop from 9 to 6g/dL. He underwent urgent endoscopy, which showed a large ulcer with a nonbleeding visible vessel and a smaller non-bleeding gastric ulcer with a clean base both in the greater curvature of the stomach. The large ulcer was treated with dual therapy. Two days later, the patient had another acute drop in Hgb to 6.5 despite being on a PPI drip. Repeat EGD was performed, which showed non-bleeding cratered gastric ulcers with pigmentation and erythematous mucosa in the antrum. The large gastric ulcer was thought to be related to cocaine use due to its specific appearance. Interestingly, his pathology was also found to be positive for H. pylori.
Discussion: From the limited literature, cocaine-associated ulcers are characterized as large with rolled edges, and thick pigmented base with eschar, similar to the ulcer identified in our case. Cocaine use accounted for approximately 36% of gastric perforations when last studied in the 1990s[1]. Many patients in this study were also positive for H pylori. This may be incidental due to the susceptible population of crack cocaine users, who are at higher risk than the general population of having H. pylori. More research needs to be done on the appearance of cocaine related ulcers and the differentiation from other peptic ulcers.
[1] Feliciano, D. V., Ojukwu, J. C., Rozycki, G. S., Ballard, R. B., Ingram, W. L., Salomone, J., Namias, N., & Newman, P. G. (1999). The epidemic of cocaine-related juxtapyloric perforations: with a comment on the importance of testing for Helicobacter pylori. Annals of surgery, 229(6), 801–806.

Disclosures:
Aakhila Rameeza, DO1, Avneet Singh, DO1, Alexander Garcia, DO1, Peter Bross, MD1, Adib Chaaya, MD2. P1407 - Cocaine-Induced Gastric Ulcers: An Under-Recognized Disease, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Cooper University Hospital, Camden, NJ; 2Cooper Medical School, Camden, NJ
Introduction: In the US, approximately 1.4 million people are affected by cocaine use disorder (CUD). Among the complications of CUD, gastric ulcer formation is less commonly identified since patients often present only after ulcer perforation. As such, gross recognition of cocaine-induced gastric ulcers often goes under recognized. Here we present the case of a patient who was found to have cocaine-induced gastric ulcers on upper endoscopy.
Case Description/Methods: A 64-year-old male with a history of CUD, hypertension and diabetes presented to the hospital for acute left-sided chest pain. He was found to have elevated troponins and new T wave inversions in anterolateral and inferior leads. Urine toxicology screen was positive for cocaine. He was started on IV heparin for NSTEMI with a plan to pursue cardiac catheterization the next day. Subsequently, he developed large volume hematemesis with a Hgb drop from 9 to 6g/dL. He underwent urgent endoscopy, which showed a large ulcer with a nonbleeding visible vessel and a smaller non-bleeding gastric ulcer with a clean base both in the greater curvature of the stomach. The large ulcer was treated with dual therapy. Two days later, the patient had another acute drop in Hgb to 6.5 despite being on a PPI drip. Repeat EGD was performed, which showed non-bleeding cratered gastric ulcers with pigmentation and erythematous mucosa in the antrum. The large gastric ulcer was thought to be related to cocaine use due to its specific appearance. Interestingly, his pathology was also found to be positive for H. pylori.
Discussion: From the limited literature, cocaine-associated ulcers are characterized as large with rolled edges, and thick pigmented base with eschar, similar to the ulcer identified in our case. Cocaine use accounted for approximately 36% of gastric perforations when last studied in the 1990s[1]. Many patients in this study were also positive for H pylori. This may be incidental due to the susceptible population of crack cocaine users, who are at higher risk than the general population of having H. pylori. More research needs to be done on the appearance of cocaine related ulcers and the differentiation from other peptic ulcers.
[1] Feliciano, D. V., Ojukwu, J. C., Rozycki, G. S., Ballard, R. B., Ingram, W. L., Salomone, J., Namias, N., & Newman, P. G. (1999). The epidemic of cocaine-related juxtapyloric perforations: with a comment on the importance of testing for Helicobacter pylori. Annals of surgery, 229(6), 801–806.

Figure: A) Large ulcer with visible non-bleeding vessel on first EGD. B) Cratered ulcer with eschar on repeat EGD
Disclosures:
Aakhila Rameeza indicated no relevant financial relationships.
Avneet Singh indicated no relevant financial relationships.
Alexander Garcia indicated no relevant financial relationships.
Peter Bross indicated no relevant financial relationships.
Adib Chaaya indicated no relevant financial relationships.
Aakhila Rameeza, DO1, Avneet Singh, DO1, Alexander Garcia, DO1, Peter Bross, MD1, Adib Chaaya, MD2. P1407 - Cocaine-Induced Gastric Ulcers: An Under-Recognized Disease, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
