Sunday Poster Session
Category: Stomach
P1411 - Severe Necrotizing Pneumonia Due to Gastropulmonary Fistula Following Roux-en-Y Gastric Bypass
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio
- HI
Humzah Iqbal, MD
University of California San Francisco, Fresno
Fresno, CA
Presenting Author(s)
Humzah Iqbal, MD1, Hunza Chaudhry, MD2, Amitpaul Gill, MD1, Juliana Yang, MD3
1University of California San Francisco, Fresno, Fresno, CA; 2University of California San Francisco, Fresno, CA; 3University of Texas Medical Branch at Galveston, Galveston, TX
Introduction: Bariatric surgery is an established treatment for severe obesity that is considered safe and effective. Gastropulmonary (GP) fistula is a rare complication. We present a unique case of necrotizing pneumonia due to a GP fistula in a patient with a history of Roux-en-Y gastric bypass (RYGB).
Case Description/Methods: A 58-year-old female with a history of laparoscopic RYGB presented with shortness of breath found to be in respiratory failure. Computed tomography (CT) imaging noted an abnormally dilated gastric remnant and the patient underwent placement of PEG tube into the remnant stomach for decompression. Respiratory and blood cultures grew vancomycin-resistant Enterococcus faecium, Klebsiella oxytoca and Escherica coli. CT abdomen with contrast injection through the PEG tube revealed a 5 cm collection of air and contrast in the left lung base and a 1.5 cm fistula between the left lung and the remnant stomach. Endoscopic treatment using single balloon was attempted but was unsuccessful due to swelling and torsion. She had multiple episodes of septic shock despite antibiotic coverage. Due to continued clinical deterioration, the patient was deemed unsuitable for surgical revision.
Discussion: RYGB accounts for 80% of bariatric surgery procedures performed in the US. Fistula formation following RYGB is rare and typically involves the gastric pouch and the gastric remnant. Fistulas with pulmonary involvement are exceedingly rare. The underlying etiology involves erosions in the intrathoracic cavity and chronic upper gastric leak. Most fistulas develop within a few months of surgery, however, our patient presented over 20 years after her RYGB. Our patient also had a unique presentation of GP fistula which presented as severe pneumonia complicated by persistent bacteremia and septic shock. The causative organisms in her infection are commonly found in the GI tract making the presence of a GP fistula the most likely underlying etiology of her pneumonia. Endoscopic management includes mechanical clips, over-the-scope clips, and endoscopic suturing, however our patient’s anatomy made endoscopic access challenging. Left lower lobectomy has been shown to be a potential surgical treatment, however further studies are needed given the rarity of the disease. Prompt evaluation is warranted in patients with a history of bariatric surgery who present with respiratory symptoms, and clinicians should be aware of GP fistula as a rare, but life-threatening complication.

Disclosures:
Humzah Iqbal, MD1, Hunza Chaudhry, MD2, Amitpaul Gill, MD1, Juliana Yang, MD3. P1411 - Severe Necrotizing Pneumonia Due to Gastropulmonary Fistula Following Roux-en-Y Gastric Bypass, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of California San Francisco, Fresno, Fresno, CA; 2University of California San Francisco, Fresno, CA; 3University of Texas Medical Branch at Galveston, Galveston, TX
Introduction: Bariatric surgery is an established treatment for severe obesity that is considered safe and effective. Gastropulmonary (GP) fistula is a rare complication. We present a unique case of necrotizing pneumonia due to a GP fistula in a patient with a history of Roux-en-Y gastric bypass (RYGB).
Case Description/Methods: A 58-year-old female with a history of laparoscopic RYGB presented with shortness of breath found to be in respiratory failure. Computed tomography (CT) imaging noted an abnormally dilated gastric remnant and the patient underwent placement of PEG tube into the remnant stomach for decompression. Respiratory and blood cultures grew vancomycin-resistant Enterococcus faecium, Klebsiella oxytoca and Escherica coli. CT abdomen with contrast injection through the PEG tube revealed a 5 cm collection of air and contrast in the left lung base and a 1.5 cm fistula between the left lung and the remnant stomach. Endoscopic treatment using single balloon was attempted but was unsuccessful due to swelling and torsion. She had multiple episodes of septic shock despite antibiotic coverage. Due to continued clinical deterioration, the patient was deemed unsuitable for surgical revision.
Discussion: RYGB accounts for 80% of bariatric surgery procedures performed in the US. Fistula formation following RYGB is rare and typically involves the gastric pouch and the gastric remnant. Fistulas with pulmonary involvement are exceedingly rare. The underlying etiology involves erosions in the intrathoracic cavity and chronic upper gastric leak. Most fistulas develop within a few months of surgery, however, our patient presented over 20 years after her RYGB. Our patient also had a unique presentation of GP fistula which presented as severe pneumonia complicated by persistent bacteremia and septic shock. The causative organisms in her infection are commonly found in the GI tract making the presence of a GP fistula the most likely underlying etiology of her pneumonia. Endoscopic management includes mechanical clips, over-the-scope clips, and endoscopic suturing, however our patient’s anatomy made endoscopic access challenging. Left lower lobectomy has been shown to be a potential surgical treatment, however further studies are needed given the rarity of the disease. Prompt evaluation is warranted in patients with a history of bariatric surgery who present with respiratory symptoms, and clinicians should be aware of GP fistula as a rare, but life-threatening complication.

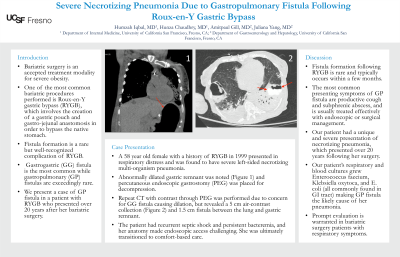
Figure: CT Chest/Abdomen with contrast through PEG tube revealing 5 cm collection of air and contrast within the left lower lobe.
Disclosures:
Humzah Iqbal indicated no relevant financial relationships.
Hunza Chaudhry indicated no relevant financial relationships.
Amitpaul Gill indicated no relevant financial relationships.
Juliana Yang indicated no relevant financial relationships.
Humzah Iqbal, MD1, Hunza Chaudhry, MD2, Amitpaul Gill, MD1, Juliana Yang, MD3. P1411 - Severe Necrotizing Pneumonia Due to Gastropulmonary Fistula Following Roux-en-Y Gastric Bypass, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
