Sunday Poster Session
Category: Stomach
P1413 - A Hard Finding to Stomach: Recurrent Acute Myeloid Leukemia Presenting as Gastric Outlet Obstruction
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio
- DS
Dipam Shah, MD
Inova Fairfax Medical Campus
Fairfax, VA
Presenting Author(s)
Dipam Shah, MD1, Monica Passi, MD2
1Inova Fairfax Medical Campus, Fairfax, VA; 2Gastro Health, Fairfax, VA
Introduction: Extramedullary infiltration (EMI) of Acute Myeloid Leukemia (AML) is rare and can be found at the time of diagnosis or during relapse. The stomach is a particularly uncommon site of EMI of AML. We present a rare case of extramedullary relapse of AML isolated to the upper GI tract.
Case Description/Methods: A 36 year old male with history of core-binding factor AML (Inv16; +c-KIT, +FLT3 KD), diagnosed 6 years ago and in remission following allogenic peripheral blood stem cell transplant presented with several weeks of post-prandial emesis, early satiety and unintentional weight loss.
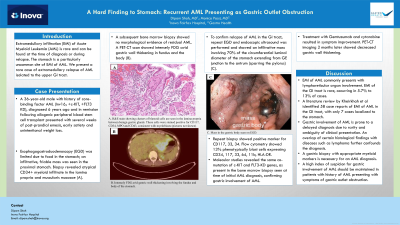
Esophagogastroduodenoscopy (EGD) was limited due to food in the stomach; an infiltrative, friable mass was seen in the proximal stomach. Biopsy revealed atypical CD34+ myeloid infiltrate in the lamina propria and muscularis mucosae (A). A subsequent bone marrow biopsy showed no morphological evidence of residual AML. A PET-CT scan showed intensely FDG avid gastric wall thickening in fundus and the body (B). To confirm relapse of AML in the GI tract, repeat EGD and endoscopic ultrasound was performed and showed an infiltrative mass involving 70% of the circumferential luminal diameter of the stomach extending from GE junction to the antrum (sparring the pylorus) (C). Repeat biopsy showed positive marker for CD117, 33, 34. Flow cytometry showed 13% phenotypically blast cells expressing CD34, 117, 33, 64, 11b, HLA-DR. Molecular studies revealed the same co-mutation of c-KIT and FLT3-KD genes, as present in the bone marrow biopsy seen at time of initial AML diagnosis, confirming gastric involvement of AML.
Treatment with Gemtuzumab and cytarabine resulted in symptom improvement. PET-CT imaging 2 months later showed decreased gastric wall thickening.
Discussion: EMI of AML commonly presents with lymphoreticular organ involvement. EMI of the GI tract is rare, occurring in 5.7% to 13% of cases. A literature review by Kheirkhah et al identified 58 case reports of EMI of AML in the GI tract, with only 7 cases localized to the stomach. Gastric involvement of AML is prone to a delayed diagnosis due to rarity and ambiguity of clinical presentation. An overlap of certain histological findings with diseases such as lymphoma further confounds the diagnosis. A gastric biopsy with appropriate myeloid markers is necessary for an AML diagnosis. A high index of suspicion for gastric involvement of AML should be maintained in patients with history of AML presenting with symptoms of gastric outlet obstruction.

Disclosures:
Dipam Shah, MD1, Monica Passi, MD2. P1413 - A Hard Finding to Stomach: Recurrent Acute Myeloid Leukemia Presenting as Gastric Outlet Obstruction, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Inova Fairfax Medical Campus, Fairfax, VA; 2Gastro Health, Fairfax, VA
Introduction: Extramedullary infiltration (EMI) of Acute Myeloid Leukemia (AML) is rare and can be found at the time of diagnosis or during relapse. The stomach is a particularly uncommon site of EMI of AML. We present a rare case of extramedullary relapse of AML isolated to the upper GI tract.
Case Description/Methods: A 36 year old male with history of core-binding factor AML (Inv16; +c-KIT, +FLT3 KD), diagnosed 6 years ago and in remission following allogenic peripheral blood stem cell transplant presented with several weeks of post-prandial emesis, early satiety and unintentional weight loss.
Esophagogastroduodenoscopy (EGD) was limited due to food in the stomach; an infiltrative, friable mass was seen in the proximal stomach. Biopsy revealed atypical CD34+ myeloid infiltrate in the lamina propria and muscularis mucosae (A). A subsequent bone marrow biopsy showed no morphological evidence of residual AML. A PET-CT scan showed intensely FDG avid gastric wall thickening in fundus and the body (B). To confirm relapse of AML in the GI tract, repeat EGD and endoscopic ultrasound was performed and showed an infiltrative mass involving 70% of the circumferential luminal diameter of the stomach extending from GE junction to the antrum (sparring the pylorus) (C). Repeat biopsy showed positive marker for CD117, 33, 34. Flow cytometry showed 13% phenotypically blast cells expressing CD34, 117, 33, 64, 11b, HLA-DR. Molecular studies revealed the same co-mutation of c-KIT and FLT3-KD genes, as present in the bone marrow biopsy seen at time of initial AML diagnosis, confirming gastric involvement of AML.
Treatment with Gemtuzumab and cytarabine resulted in symptom improvement. PET-CT imaging 2 months later showed decreased gastric wall thickening.
Discussion: EMI of AML commonly presents with lymphoreticular organ involvement. EMI of the GI tract is rare, occurring in 5.7% to 13% of cases. A literature review by Kheirkhah et al identified 58 case reports of EMI of AML in the GI tract, with only 7 cases localized to the stomach. Gastric involvement of AML is prone to a delayed diagnosis due to rarity and ambiguity of clinical presentation. An overlap of certain histological findings with diseases such as lymphoma further confounds the diagnosis. A gastric biopsy with appropriate myeloid markers is necessary for an AML diagnosis. A high index of suspicion for gastric involvement of AML should be maintained in patients with history of AML presenting with symptoms of gastric outlet obstruction.

Figure: A. H&E stain from gastric biopsy showing clusters of blastoid cells are seen in the lamina propria between benign gastric glands. These cells were stained positive for CD117, CD34, MPO and CD43, consistent with myeloblasts (pictures not shown-o7).
B. PET-CT demonstrating intensely FDG avid gastric wall thickening involving the fundus and the body of stomach.
C. Endoscopy demonstrating an infiltrative mass in the gastric body.
B. PET-CT demonstrating intensely FDG avid gastric wall thickening involving the fundus and the body of stomach.
C. Endoscopy demonstrating an infiltrative mass in the gastric body.
Disclosures:
Dipam Shah indicated no relevant financial relationships.
Monica Passi indicated no relevant financial relationships.
Dipam Shah, MD1, Monica Passi, MD2. P1413 - A Hard Finding to Stomach: Recurrent Acute Myeloid Leukemia Presenting as Gastric Outlet Obstruction, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
