Sunday Poster Session
Category: Stomach
P1375 - Gastric Mucormycosis in an Immunosuppressed Patient Following Dual Pancreas-Kidney Transplant
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio
.jpg)
Jang Hyun Kim, MD
Montefiore Medical Center
Presenting Author(s)
Jang Hyun Kim, MD, Diana Wee, MD, Daniel Behin, MD, Lawrence Brandt, MD, MACG
Montefiore Medical Center, Bronx, NY
Introduction: Mucormycosis is a highly invasive disease caused by fungi in the Mucorales order. Cases of gastrointestinal mucormycosis have been rising over the past few decades. We present a case of gastric mucormycosis found on endoscopic evaluation.
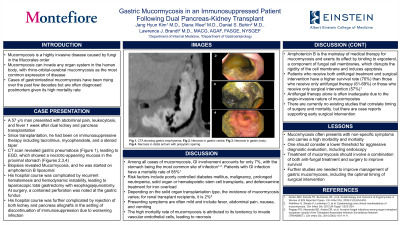
Case Description/Methods: We present a 57-year-old man with hypertension and type I diabetes mellitus who had a dual kidney and pancreas transplant one week prior to presentation. After starting immunosuppressive therapy, he was found to have persistent abdominal pain and vomiting in the setting of a new leukocytosis and fever. After undergoing a CT of the abdomen and pelvis, gastric pneumatosis was seen (Figure 1). An esophagogastroduodenoscopy was done, showing necrotic-appearing mucosa of the stomach (Figures 2,3,4). Biopsies showed Mucormycosis. Patient’s immunosuppression, except glucocorticoids, were discontinued, and he was immediately started on amphotericin B liposomal.
Two weeks later, the patient’s course was complicated by hematemesis. He underwent a laparoscopic total gastrectomy with Roux-en-Y esophagojejunostomy. Intra-operatively, he was noted to have a contained perforation of the stomach fundus. Histologic examination of the resected stomach showed mucormycosis with necrosis.
Discussion: Gastrointestinal mucormycosis is rare with the stomach being the most common site of infection, which carries a high mortality rate. In our patient, the most likely cause was his immunosuppressive state after organ transplantation. Mucormycosis’ high mortality rate is attributed to its tendency to invade endothelial cells of the vascular system. Due to non-specific symptoms, diagnosis is often delayed.
Amphotericin B is the mainstay of medical therapy for mucormycosis, but it can be inadequate due to poor penetration of antifungal agents at the sites of infection. Surgical intervention with medical therapy increases the survival rate. Although there are no existing studies that correlate timing of surgery and mortality, there are case reports that support early surgical intervention.
In conclusion, mucormycosis carries a high morbidity and mortality. Thus, there should be a lower threshold for aggressive diagnostic evaluation, including endoscopy, when appropriate. In addition, treatment of mucormycosis should involve a combination of both antifungal therapy and surgery to improve survival. Further studies are needed to improve management of gastric mucormycosis, including the optimal timing of surgical intervention.

Disclosures:
Jang Hyun Kim, MD, Diana Wee, MD, Daniel Behin, MD, Lawrence Brandt, MD, MACG. P1375 - Gastric Mucormycosis in an Immunosuppressed Patient Following Dual Pancreas-Kidney Transplant, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Montefiore Medical Center, Bronx, NY
Introduction: Mucormycosis is a highly invasive disease caused by fungi in the Mucorales order. Cases of gastrointestinal mucormycosis have been rising over the past few decades. We present a case of gastric mucormycosis found on endoscopic evaluation.
Case Description/Methods: We present a 57-year-old man with hypertension and type I diabetes mellitus who had a dual kidney and pancreas transplant one week prior to presentation. After starting immunosuppressive therapy, he was found to have persistent abdominal pain and vomiting in the setting of a new leukocytosis and fever. After undergoing a CT of the abdomen and pelvis, gastric pneumatosis was seen (Figure 1). An esophagogastroduodenoscopy was done, showing necrotic-appearing mucosa of the stomach (Figures 2,3,4). Biopsies showed Mucormycosis. Patient’s immunosuppression, except glucocorticoids, were discontinued, and he was immediately started on amphotericin B liposomal.
Two weeks later, the patient’s course was complicated by hematemesis. He underwent a laparoscopic total gastrectomy with Roux-en-Y esophagojejunostomy. Intra-operatively, he was noted to have a contained perforation of the stomach fundus. Histologic examination of the resected stomach showed mucormycosis with necrosis.
Discussion: Gastrointestinal mucormycosis is rare with the stomach being the most common site of infection, which carries a high mortality rate. In our patient, the most likely cause was his immunosuppressive state after organ transplantation. Mucormycosis’ high mortality rate is attributed to its tendency to invade endothelial cells of the vascular system. Due to non-specific symptoms, diagnosis is often delayed.
Amphotericin B is the mainstay of medical therapy for mucormycosis, but it can be inadequate due to poor penetration of antifungal agents at the sites of infection. Surgical intervention with medical therapy increases the survival rate. Although there are no existing studies that correlate timing of surgery and mortality, there are case reports that support early surgical intervention.
In conclusion, mucormycosis carries a high morbidity and mortality. Thus, there should be a lower threshold for aggressive diagnostic evaluation, including endoscopy, when appropriate. In addition, treatment of mucormycosis should involve a combination of both antifungal therapy and surgery to improve survival. Further studies are needed to improve management of gastric mucormycosis, including the optimal timing of surgical intervention.

Figure: Figure 1. Non-contrast CT scan of the abdomen showing gastric emphysema. Figure 2. Endoscopic image of the gastric cardia showing necrosis. Figure 3. Endoscopic image of the gastric body showing necrosis. Figure 4. Endoscopic image of the gastric antrum that shows necrosis in the distal antrum and sparing of the prepyloric region.
Disclosures:
Jang Hyun Kim indicated no relevant financial relationships.
Diana Wee indicated no relevant financial relationships.
Daniel Behin indicated no relevant financial relationships.
Lawrence Brandt: Ferring Pharmaceuticals – Advisor or Review Panel Member, Consultant.
Jang Hyun Kim, MD, Diana Wee, MD, Daniel Behin, MD, Lawrence Brandt, MD, MACG. P1375 - Gastric Mucormycosis in an Immunosuppressed Patient Following Dual Pancreas-Kidney Transplant, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
