Sunday Poster Session
Category: Stomach
P1388 - A Case Series: Early Gastric Outlet Obstruction Secondary to Intragastric Balloon Placement
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio

Alexa Trovato, MD
Boston Medical Center
Boston, MA
Presenting Author(s)
Alexa Trovato, MD1, Matthew J. Custodio, MD1, Julia Ding, MD1, Madeleine Haff, MD1, David Lichtenstein, MD2, Laura Chiu, MD, MPH3
1Boston Medical Center, Boston, MA; 2Boston Medical Center, Boston University School of Medicine, Boston, MA; 3Boston University Medical Center, Boston, MA
Introduction: Intragastric balloon therapy is a minimally invasive, non-surgical restrictive weight loss procedure that promotes early satiety and delayed gastric emptying, resulting in reduced caloric intake. Common adverse effects include nausea, vomiting, abdominal pain, and reflux. More serious adverse effects are rare, and include balloon migration, gastric ulceration and perforation, and acute pancreatitis.
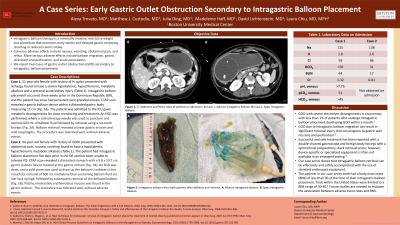
Case Description/Methods: We report two cases of 44- and 51-year-old females who both presented with intractable nausea and vomiting, severe hypokalemia (1.8-2.6 mmol/L), and hypochloremic metabolic alkalosis secondary to gastric outlet obstruction (GOO) after intragastric balloon placement (Table 1). Both intragastric balloons were placed in the Dominican Republic five days (Spatz System) and three weeks (Allurion balloon) prior to hospital presentation. After immediate nasogastric decompression and fluid resuscitation, both patients underwent successful removal of the intragastric balloons via esophagogastroduodenoscopy. A sclerotherapy needle was used to aspirate the Allurion balloon fluid followed by retrieval using a rat-tooth forceps. A snare was used to draw up the catheter from the Spatz balloon prior to aspirating its fluid and subsequent retrieval of the deflated balloon (Fig. 1). Approximately 500-600 mL of fluid from each balloon was aspirated. Balloon retrieval revealed a linear gastric erosion and mild esophagitis in one patient. Both patients tolerated the procedure well with no complications.
Discussion: Gastric outlet obstruction with severe electrolyte derangements is an uncommon, but serious adverse effect of intragastric balloon therapy that should be recognized to prevent progression to gastric wall necrosis and perforation. Studies reveal that fewer than 1% of patients who undergo intragastric balloon placement suffer from GOO within one month. Limited cases have been reported on using endoscopic balloon deflation and retrieval for GOO secondary to intragastric balloon placement. While it may be preferred to utilize retrieval equipment specific to each intragastric balloon device, one observational study has shown that using a double-channel gastroscope and foreign body forceps plus symmetrical polypectomy shark retrieval snare is both efficacious and safe. Our case series further demonstrates that the use of standard endoscopic equipment can also be safe and effective for intragastric balloon retrieval.

Disclosures:
Alexa Trovato, MD1, Matthew J. Custodio, MD1, Julia Ding, MD1, Madeleine Haff, MD1, David Lichtenstein, MD2, Laura Chiu, MD, MPH3. P1388 - A Case Series: Early Gastric Outlet Obstruction Secondary to Intragastric Balloon Placement, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Boston Medical Center, Boston, MA; 2Boston Medical Center, Boston University School of Medicine, Boston, MA; 3Boston University Medical Center, Boston, MA
Introduction: Intragastric balloon therapy is a minimally invasive, non-surgical restrictive weight loss procedure that promotes early satiety and delayed gastric emptying, resulting in reduced caloric intake. Common adverse effects include nausea, vomiting, abdominal pain, and reflux. More serious adverse effects are rare, and include balloon migration, gastric ulceration and perforation, and acute pancreatitis.
Case Description/Methods: We report two cases of 44- and 51-year-old females who both presented with intractable nausea and vomiting, severe hypokalemia (1.8-2.6 mmol/L), and hypochloremic metabolic alkalosis secondary to gastric outlet obstruction (GOO) after intragastric balloon placement (Table 1). Both intragastric balloons were placed in the Dominican Republic five days (Spatz System) and three weeks (Allurion balloon) prior to hospital presentation. After immediate nasogastric decompression and fluid resuscitation, both patients underwent successful removal of the intragastric balloons via esophagogastroduodenoscopy. A sclerotherapy needle was used to aspirate the Allurion balloon fluid followed by retrieval using a rat-tooth forceps. A snare was used to draw up the catheter from the Spatz balloon prior to aspirating its fluid and subsequent retrieval of the deflated balloon (Fig. 1). Approximately 500-600 mL of fluid from each balloon was aspirated. Balloon retrieval revealed a linear gastric erosion and mild esophagitis in one patient. Both patients tolerated the procedure well with no complications.
Discussion: Gastric outlet obstruction with severe electrolyte derangements is an uncommon, but serious adverse effect of intragastric balloon therapy that should be recognized to prevent progression to gastric wall necrosis and perforation. Studies reveal that fewer than 1% of patients who undergo intragastric balloon placement suffer from GOO within one month. Limited cases have been reported on using endoscopic balloon deflation and retrieval for GOO secondary to intragastric balloon placement. While it may be preferred to utilize retrieval equipment specific to each intragastric balloon device, one observational study has shown that using a double-channel gastroscope and foreign body forceps plus symmetrical polypectomy shark retrieval snare is both efficacious and safe. Our case series further demonstrates that the use of standard endoscopic equipment can also be safe and effective for intragastric balloon retrieval.

Figure: Figure 1. Intragastric Balloons From Both Patients After Deflation and Retrieval. Left is Allurion Intragastric Balloon and Right is Spatz Intragastric Balloon.
| Patient 1 | Patient 2 | |
| Na | 125 | 138 |
| K | 1.8 | 2.6 |
| Cl | 59 | 96 |
| HCO3 | >50 | 31 |
| BUN | 43 | 17 |
| Cr | 1.43 | 0.81 |
| pH | > 7.75 | Not Collected |
| pCO2 | 51 | Not Collected |
Table: Table 1. Laboratory values of each patient on admission and prior to significant resuscitation.
Disclosures:
Alexa Trovato indicated no relevant financial relationships.
Matthew Custodio indicated no relevant financial relationships.
Julia Ding indicated no relevant financial relationships.
Madeleine Haff indicated no relevant financial relationships.
David Lichtenstein: ABIM – GI board committee. Ambu – Consultant. Boston Scientific Inc – Consultant. Elements Endoscopy – Advisor or Review Panel Member. Iterative Health – Advisory Committee/Board Member, Grant/Research Support. Olympus – Consultant, Speakers Bureau. Palette Life Sciences – Clinical events committee. SafeHeal – Advisory Committee/Board Member.
Laura Chiu indicated no relevant financial relationships.
Alexa Trovato, MD1, Matthew J. Custodio, MD1, Julia Ding, MD1, Madeleine Haff, MD1, David Lichtenstein, MD2, Laura Chiu, MD, MPH3. P1388 - A Case Series: Early Gastric Outlet Obstruction Secondary to Intragastric Balloon Placement, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
