Sunday Poster Session
Category: Liver
P1148 - Idiopathic Non-Cirrhotic Portal Hypertension With Type B Hepatic Encephalopathy Due to Obliterative Portal Venopathy Secondary to Systemic Lupus Erythematosus and Mixed Connective Tissue Disease
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall
Has Audio
.jpg)
Makeda Dawkins, MD
Westchester Medical Center
Valhalla, NY
Presenting Author(s)
Makeda Dawkins, MD, Michael Rosman, MD, Bernard Partiula, DO
Westchester Medical Center, Valhalla, NY
Introduction: Non-cirrhotic portal hypertension (NCPH) refers to diseases with the propensity to increase portal pressure without underlying liver fibrosis. The rarest cause is idiopathic portal hypertension (IPH), associated with immunologic and genetic disorders, chronic infections, and prothrombotic conditions. We present a case of idiopathic portal hypertension secondary to obliterative portal venopathy (OPV) in the setting of systemic lupus erythematosus (SLE) and mixed connective disease (MCTD).
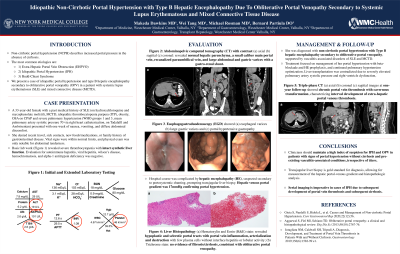
Case Description/Methods: A 33-year-old female with SLE, MCTD, idiopathic thrombocytopenia purpura, and pulmonary hypertension (mPAP 70) presented with vomiting and diffuse abdominal pain for a week without recent travel, sick contacts, or new foods/medications. Vital signs were within normal limits, and physical exam noted diffuse abdominal tenderness. Lab work showed severe thrombocytopenia and preserved synthetic liver function without transaminitis or hyperbilirubinemia. Abdominal CT showed normal hepatic parenchyma, a small main portal vein, gastric varices, recanalized umbilical vein, and a gastro-renal shunt. She developed hepatic encephalopathy (HE) type B from portosystemic shunting. Liver biopsy was performed to assess portal hypertension and identify any underlying disease, as imaging and serologies failed to elucidate a diagnosis. Histopathology showed hypoplastic sclerotic portal tracts and lymphocytic portal vein destruction without fibrosis (Figure 1), confirming non-cirrhotic idiopathic portal hypertension due to obliterative portal venopathy, supported by her vasculitis-associated disorders of SLE and MCTD. Serial CT showed portal vein thrombosis and cavernous transformation, highlighting interval development of secondary extrahepatic portal vein obstruction in patients with IPH. Severe thrombocytopenia prohibited anticoagulation. HE prophylaxis and pulmonary hypertension treatment were prioritized to ensure liver transplant candidacy in light of anticipated cirrhosis development.
Discussion: Non-cirrhotic portal hypertension describes increased portal pressure in absence of cirrhosis. Visualized portal vein destruction with sclerosis on histopathology should raise concern for obliterative portal venopathy. Clinicians should maintain a high index of suspicion for IPH secondary to OPV in patients with vasculitis-associated rheumatologic disorders, namely SLE and MCTD, and attain follow-up imaging to monitor for long-term complications, including portal vein thrombosis and subsequent cirrhosis.

Disclosures:
Makeda Dawkins, MD, Michael Rosman, MD, Bernard Partiula, DO. P1148 - Idiopathic Non-Cirrhotic Portal Hypertension With Type B Hepatic Encephalopathy Due to Obliterative Portal Venopathy Secondary to Systemic Lupus Erythematosus and Mixed Connective Tissue Disease, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Westchester Medical Center, Valhalla, NY
Introduction: Non-cirrhotic portal hypertension (NCPH) refers to diseases with the propensity to increase portal pressure without underlying liver fibrosis. The rarest cause is idiopathic portal hypertension (IPH), associated with immunologic and genetic disorders, chronic infections, and prothrombotic conditions. We present a case of idiopathic portal hypertension secondary to obliterative portal venopathy (OPV) in the setting of systemic lupus erythematosus (SLE) and mixed connective disease (MCTD).
Case Description/Methods: A 33-year-old female with SLE, MCTD, idiopathic thrombocytopenia purpura, and pulmonary hypertension (mPAP 70) presented with vomiting and diffuse abdominal pain for a week without recent travel, sick contacts, or new foods/medications. Vital signs were within normal limits, and physical exam noted diffuse abdominal tenderness. Lab work showed severe thrombocytopenia and preserved synthetic liver function without transaminitis or hyperbilirubinemia. Abdominal CT showed normal hepatic parenchyma, a small main portal vein, gastric varices, recanalized umbilical vein, and a gastro-renal shunt. She developed hepatic encephalopathy (HE) type B from portosystemic shunting. Liver biopsy was performed to assess portal hypertension and identify any underlying disease, as imaging and serologies failed to elucidate a diagnosis. Histopathology showed hypoplastic sclerotic portal tracts and lymphocytic portal vein destruction without fibrosis (Figure 1), confirming non-cirrhotic idiopathic portal hypertension due to obliterative portal venopathy, supported by her vasculitis-associated disorders of SLE and MCTD. Serial CT showed portal vein thrombosis and cavernous transformation, highlighting interval development of secondary extrahepatic portal vein obstruction in patients with IPH. Severe thrombocytopenia prohibited anticoagulation. HE prophylaxis and pulmonary hypertension treatment were prioritized to ensure liver transplant candidacy in light of anticipated cirrhosis development.
Discussion: Non-cirrhotic portal hypertension describes increased portal pressure in absence of cirrhosis. Visualized portal vein destruction with sclerosis on histopathology should raise concern for obliterative portal venopathy. Clinicians should maintain a high index of suspicion for IPH secondary to OPV in patients with vasculitis-associated rheumatologic disorders, namely SLE and MCTD, and attain follow-up imaging to monitor for long-term complications, including portal vein thrombosis and subsequent cirrhosis.

Figure: Figure 1: Liver Histopathology: (a) Hematoxylin and Eosin (H&E) stain revealing hypoplastic and sclerotic portal tracts with portal vein inflammation, arterialization and destruction with few plasma cells without interface hepatitis or lobular activity; (b) Trichrome stain without no evidence of fibrosis or cirrhosis, consistent with obliterative portal venopathy.
Disclosures:
Makeda Dawkins indicated no relevant financial relationships.
Michael Rosman indicated no relevant financial relationships.
Bernard Partiula indicated no relevant financial relationships.
Makeda Dawkins, MD, Michael Rosman, MD, Bernard Partiula, DO. P1148 - Idiopathic Non-Cirrhotic Portal Hypertension With Type B Hepatic Encephalopathy Due to Obliterative Portal Venopathy Secondary to Systemic Lupus Erythematosus and Mixed Connective Tissue Disease, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
