Sunday Poster Session
Category: Liver
P1149 - Neuro-Pulmonary Syndrome Secondary to Invasive Fungal Infection After One Year of a Liver Transplant, a Stroke Mimicker
Sunday, October 22, 2023
3:30 PM - 7:00 PM PT
Location: Exhibit Hall

Hilary A. Elom, MD, MPH
University of Mississippi Medical Center
Columbia, MO
Presenting Author(s)
Hilary A. Elom, MD, MPH, Ismail Ganim, MD, Anna Owings, DO
University of Mississippi Medical Center, Jackson, MS
Introduction: Liver transplantation has revolutionized the management of end-stage liver diseases and acute liver failure globally, with a survival rate of 90% at one year and 80% at five years. Improved preoperative evaluation, techniques, and postoperative immunosuppressive medication are all factors in liver transplant success. However, one of the risks of immunosuppression is the propensity for posttransplant infections with associated morbidity and mortality, although usually within the first two months of transplant. Here, we present a unique case of invasive fungal infection after one year of liver transplantation.
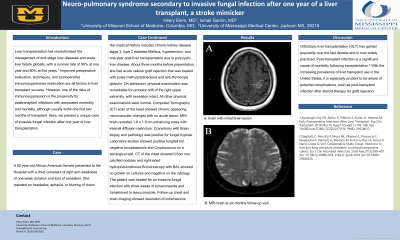
Case Description/Methods: A 52-year-old African American female presented to the Hospital with a chief complaint of right arm weakness of one-week duration and loss of sensation. She reported no headache, aphasia, or blurring of vision. Her medical history includes chronic kidney disease stage 3, type 2 diabetes Mellitus, hypertension, and one-year post-liver transplantation due to polycystic liver disease. About three months before presentation, she had acute cellular graft rejection that was treated with pulse methylprednisolone and anti-thymocyte globulin. On admission, physical examination was remarkable for pronator drift of the right upper extremity, with sensation intact. All other physical examinations were normal. Computed Tomography (CT) scan of the head showed chronic appearing microvascular changes with no acute lesion. MRI brain revealed 1.6 x 1.8 cm enhancing mass with internal diffusion restriction. Craniotomy with Brain biopsy and pathology was positive for fungal hyphae. Laboratory studies showed positive fungitell but negative toxoplasmosis and Cryptococcus on a serological test. CT of the chest showed 0.5cm non-calcified nodules and right-sided hydropneumothorax. Bronchoscopy with BAL showed no growth on cultures and negative on the cytology. The patient was treated for an invasive fungal infection with three weeks of posaconazole and transitioned to isavuconazole. Follow-up chest and brain imaging showed resolution of initial lesions.
Discussion: Orthotopic liver transplantation (OLT) has gained popularity over the last decade and is now widely practiced. Post-transplant infection is a significant cause of morbidity following transplantation. With the increasing prevalence of liver transplant use in the United States, it is especially prudent to be aware of potential complications, such as post-transplant infection after steroid therapy for graft rejection.

Disclosures:
Hilary A. Elom, MD, MPH, Ismail Ganim, MD, Anna Owings, DO. P1149 - Neuro-Pulmonary Syndrome Secondary to Invasive Fungal Infection After One Year of a Liver Transplant, a Stroke Mimicker, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
University of Mississippi Medical Center, Jackson, MS
Introduction: Liver transplantation has revolutionized the management of end-stage liver diseases and acute liver failure globally, with a survival rate of 90% at one year and 80% at five years. Improved preoperative evaluation, techniques, and postoperative immunosuppressive medication are all factors in liver transplant success. However, one of the risks of immunosuppression is the propensity for posttransplant infections with associated morbidity and mortality, although usually within the first two months of transplant. Here, we present a unique case of invasive fungal infection after one year of liver transplantation.
Case Description/Methods: A 52-year-old African American female presented to the Hospital with a chief complaint of right arm weakness of one-week duration and loss of sensation. She reported no headache, aphasia, or blurring of vision. Her medical history includes chronic kidney disease stage 3, type 2 diabetes Mellitus, hypertension, and one-year post-liver transplantation due to polycystic liver disease. About three months before presentation, she had acute cellular graft rejection that was treated with pulse methylprednisolone and anti-thymocyte globulin. On admission, physical examination was remarkable for pronator drift of the right upper extremity, with sensation intact. All other physical examinations were normal. Computed Tomography (CT) scan of the head showed chronic appearing microvascular changes with no acute lesion. MRI brain revealed 1.6 x 1.8 cm enhancing mass with internal diffusion restriction. Craniotomy with Brain biopsy and pathology was positive for fungal hyphae. Laboratory studies showed positive fungitell but negative toxoplasmosis and Cryptococcus on a serological test. CT of the chest showed 0.5cm non-calcified nodules and right-sided hydropneumothorax. Bronchoscopy with BAL showed no growth on cultures and negative on the cytology. The patient was treated for an invasive fungal infection with three weeks of posaconazole and transitioned to isavuconazole. Follow-up chest and brain imaging showed resolution of initial lesions.
Discussion: Orthotopic liver transplantation (OLT) has gained popularity over the last decade and is now widely practiced. Post-transplant infection is a significant cause of morbidity following transplantation. With the increasing prevalence of liver transplant use in the United States, it is especially prudent to be aware of potential complications, such as post-transplant infection after steroid therapy for graft rejection.

Figure: A: brain with initial brain lesion and B: MRI brain at six months follow-up visit
Disclosures:
Hilary Elom indicated no relevant financial relationships.
Ismail Ganim indicated no relevant financial relationships.
Anna Owings indicated no relevant financial relationships.
Hilary A. Elom, MD, MPH, Ismail Ganim, MD, Anna Owings, DO. P1149 - Neuro-Pulmonary Syndrome Secondary to Invasive Fungal Infection After One Year of a Liver Transplant, a Stroke Mimicker, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
